IS MAJOR PANCREATIC SURGERY FEASIBLE AND SAFE IN PATIENTS WHO REFUSE BLOOD TRANSFUSION? SINGLE-INSTITUTION EXPERIENCE WITH 32 CONSECUTIVE JEHOVAH'S WITNESSES PATIENTS
Mario De Bellis*, Andrea Ruzzenente, Fabio Bagante, Raffaele Ziello, Tommaso Campagnaro, Simone Conci, Filippo Nifosi', Ezio Lombardo, Giovanni Lazzari, Alfredo Guglielmi, Calogero Iacono
Surgery, University of Verona, Verona, Italy
Background. The refusal of blood transfusion for surgical procedures at high risk of bleeding, such as major pancreatic resection, forces surgeons to face ethical challenges and raises concerns about appropriate perioperative management. A single-institution experience was reviewed to assess feasibility and short-term outcomes of bloodless major pancreatic surgery.
Methods. The institutional database was retrospectively reviewed to identify patients undergoing curative surgery for pancreatic and periampullary tumors from January 2010 through August 2018. A protocol to optimize perioperative hemoglobin (Hb) values by administration of drugs stimulating erythropoiesis and to minimize blood loss was systematically used. This protocol was designed to reduce the need for allogeneic blood transfusions and improve patient outcomes.
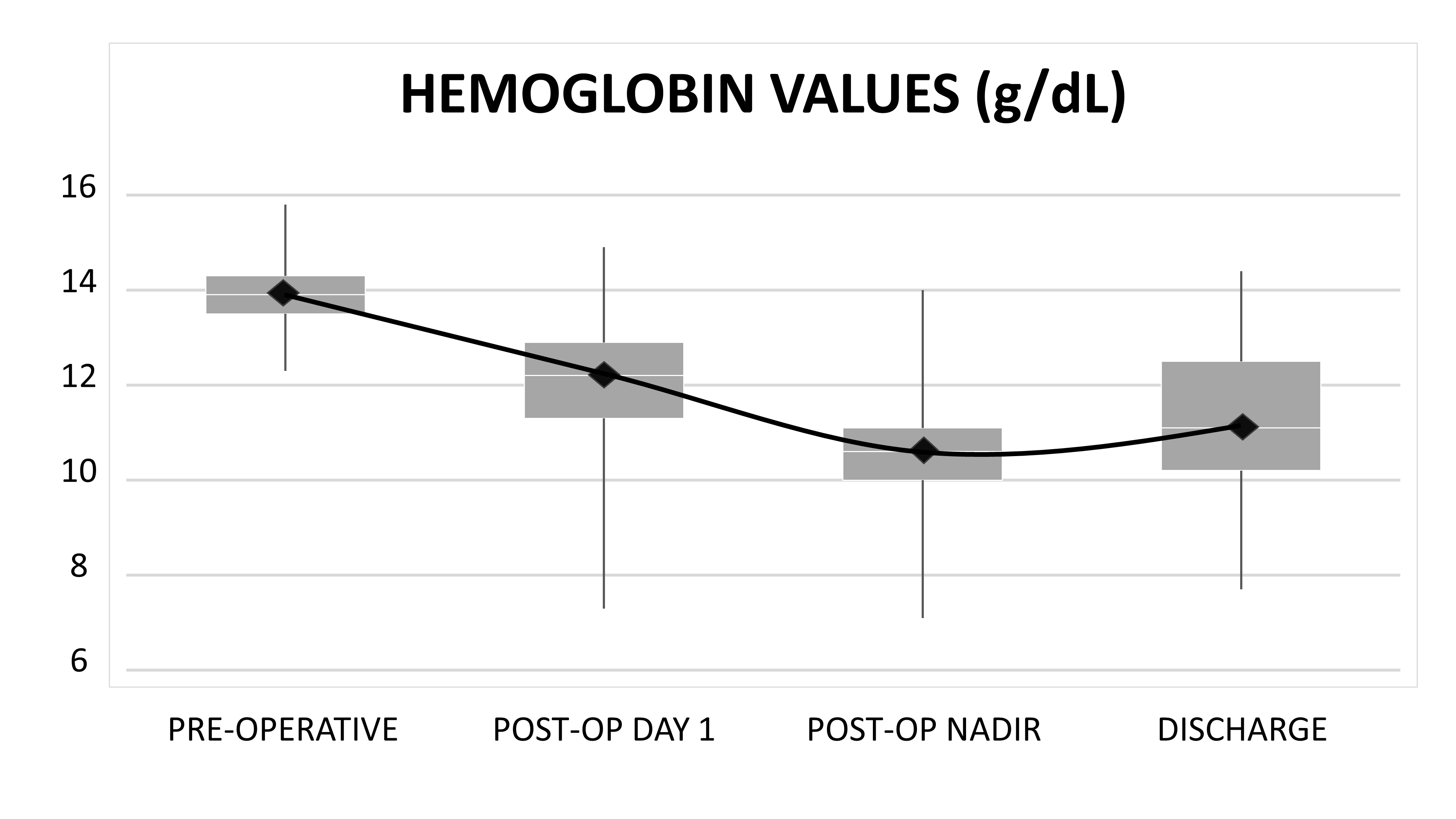
Results. Perioperative outcomes of 32 JW patients were included. Median age was 67 years (range, 31-77) and 19 (59.4%) patients were treated with preoperative erythropoietin. Five (15.6%) patients had a medical history of previous abdominal surgery while 4 (12.5%) patients were treated with neoadjuvant chemotherapy for borderline resectable pancreatic duct adenocarcinoma (PDAC). Twenty-four (75%) patients underwent pancreaticoduodenectomy, 4 (12.5%) distal pancreatectomy (DP) with splenectomy, 3 (9.4%) spleen-preserving DP, and 1 (3.1%) total pancreatectomy. No cases required vascular resection and median time of surgery was 470 minutes (range, 290-595). Median estimated intraoperative blood loss was 400 mL (range, 100-1000) and cell saver has never been used. Median preoperative Hb was 13.9 g/dL (range, 11.7-15.8) while median postoperative nadir Hb was 10.5 g/dL (range, 7.1-14.1). Although median Hb level decreased of 2.8 g/dL (range, 0-6.9) during the postoperative course, its level rose to 11.1 g/dL (range, 7.7-14.4) at discharge. The median number of lymph nodes harvested for all malignant neoplasms was 23 (range. 14-50). The most common histological diagnosis (n=15, 46.9%) was PDAC. Clavien-Dindo grade I-II complications occurred in 14 patients (43.8%): 5 (15.6%) postoperative pancreatic fistula (POPF) grade A, 1 (3.1%) POPF grade B, 2 (6.3%) delayed gastric emptying, 2 (6.3%) biliary fistulas, and 1 (3.1%) pulmonary thromboembolism. Only 1 (3.1%) patient had a Clavien-Dindo grade III complication, which was an abdominal fluid collection that required percutaneous drainage. Median length of stay was 16 days (range, 8-54) with no patient requiring transfusion or re-operation and no 90-day mortality.
Conclusions. A multidisciplinary approach and specific perioperative management allowed to perform major pancreatic surgery in JW patients with good short-term outcomes. Long-term results should be assessed with particular attention to disease progression following perioperative treatment with erythropoiesis-stimulating agents.
Review of current literature on major pancreatic surgery in Jehovah's Witness patients
| Cases | Period (years) | Pancreatic resection | Hb pre-op | ABT | Morbidity | Mortality | |
| Konstantinidis (2013) | 10 | 15 | 6 PD 4 DP/SP | 12.5 | 1 | 25 | 0 |
| Lee (2016) | 11 | 7 | 4 PPPD 4 PD 2 SP 1 DP | 12.5 | 0 | 36 | 0 |
| Present study (2018) | 32 | 8 | 24 PPPD 4 DP 3 SP 1 TP | 13.9 | 0 | 47 | 0 |
ABT = allogenic blood transfusion, PD = pancreaticoduodenectomy, DP = distal pancreatectomy with splenectomy, SP = spleen-preserving distal pancreatectomy, PPPD = pylorus-preserving pancreaticoduodenectomy, TP = total pancreatectomy.
Back to 2019 Posters




