THERMAL INJURY FROM RADIOFREQUENCY CATHETER ABLATION FOR ATRIAL FIBRILLATION AS RISK FACTOR FOR ESOPHAGEAL SQUAMOUS CELL CARCINOMA: A CASE REPORT
Shahin Ayazi1, Kristy Chovanec*1, Brian S. Goodman2, Fahim Habib1, Ali H. Zaidi1, Blair A. Jobe1
1Esophageal and Lung Institute, Allegheny Health Network, Pittsburgh, PA; 2Radiology, Allegheny Health Network, Pittsburgh, PA
Introduction:
Radiofrequency catheter ablation is increasingly used in the treatment of atrial fibrillation (AFib). Collateral thermal damage to the adjacent structures particularly to the esophagus is a known complication of this procedure. In this report, we present a case who developed squamous cell carcinoma (SCC) of the esophagus 7 years after thermal injury to the esophagus during a catheter ablation for treatment of AFib.
Case Presentation:
In our case, we present a 64-year-old white male who underwent a pulmonary vein isolation (PVI) radiofrequency ablation in 2011. This procedure was aborted due to thermal injury to the esophagus. He resumed pharmacological management for his AFib and eventually underwent another PVI ablation 6 years later. This procedure was successful, and his cardiac arrhythmia was resolved. In Early 2018, he started to experience some substernal pain and discomfort during eating. He was started on PPI with partial improvement, but with worsening of his symptoms, an upper endoscopy was performed to further evaluate his foregut symptoms. On Endoscopy, he was found to have a diffuse erythematous area of about 5 cm in the lower third of the esophagus (35-40 cm from incisors) with mucosal irregularity and erosion. Biopsies from this area revealed poorly differentiated squamous cell carcinoma. The patient was then referred to our institution for further management. During our evaluation, he denied any personal or family history of foregut malignancies or any gastrointestinal disease. The patient has not had any exposures to environmental toxins and denied alcohol or tobacco use. He underwent clinical staging and was found to be T2N0M0. He then underwent a minimally invasive Ivor Lewis esophagectomy. The surgery and postoperative course were uneventful, he was discharged on postoperative day 7 and surgical pathology returned as T1aN0.
Conclusion:
Given the lack of any of previously described risk factors for esophageal SCC in this case, it may be worth considering this cancer case as one originating from the thermal injury that occurred during AFib ablation. Review of the imaging of the patient also demonstrates that the location of the cancer is matching the site of thermal injury (Figure). Mechanical and chemical injury to the esophagus are known risk factors for developing squamous cell carcinoma of the esophagus. Studies have suggested that following ablation for AFib, up to 47% of patients have some degree of esophageal mucosal changes suggestive for thermal injuries and in up to 18% there is evidence of necrosis or ulcer-like changes. This case is the first that raises the concern that these thermal injuries can lead to a neoplastic process and prompts a low threshold for endoscopic evaluation of patients with foregut symptoms and previous thermal injury during AFib ablation.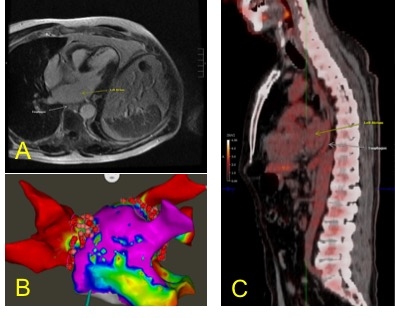
(A) MRI angiogram of the patient prior to the second PVI demonstrating proximity of the distal esophagus to the posterior left atrial endocardium, the site used for ablation during PVI. (B) The electroanatomic map of the left atrium of this patient during PVI procedure, the ablated area is in close contact with esophagus. (C) PET/CT demonstrating an area with hypermetabolic activity at the site of biopsy proven cancer in the distal esophagus, posterior to the left atrium.
Back to 2019 Posters




