ROBOTIC FUNDOPLICATIONS FOR GIANT PARAESOPHAGEAL HERNIA: ROLE OF BIOSYNTHETIC TISSUE REINFORCEMENT AFTER CRUROPLASTY
Massimo Arcerito*1,2, Harpreet Kaur3, John T. Moon4
1Surgery, University of California Riversdie, Riverside, CA; 2Surgery, Riverside Community Hospital, Riverside, California, CA; 3School of Medicine, Government Medical College, Patiala, India; 4Surgery, Shawnee Mission Medical Center, Overland Park, KS
Introduction. Minimally invasive technique has a well defined role in treating gastroesophageal reflux disease and small hiatal hernias. Large paraesophageal hernias constitute a surgical challenge, and robotic surgery is still considered a novel approach in their treatment. Hypothesis. We hypothesized the use of biosynthetic mesh in reinforcing the cruroplasty as a mandatory adjuvant technique to robotic fundoplication, while treating large paraesophageal hiatal hernias. Material and Methods. Between March 2014 and March 2018, 70 patients (23 males, 47 females) with mean age of 64 (22-92) and giant paraesophageal hernia, by radiographic criteria, underwent robotic fundoplication with biosynthetic tissue reinforcement mesh. All patients underwent upper endoscopy and upper gastrointestinal series. Esophageal manometry and pH monitoring were performed in 42 patients. Emergent surgery, operative time, intra- and perioperative complications, hospital stay, short and long clinical outcome, postoperative dysphagia and mesh related complications represented main outcome measures in our prospective study. Follow up was obtained at 14, 30, 90 days and yearly thereafter. Results. Eleven patients presented with acute onset of symptoms (8 severe gastric outlet obstruction and 3 hematemesis due to Cameron ulcer). Heartburn was present in 36%, regurgitation in 70%, dysphagia in 80%, respiratory symptoms in 90%. All patients were completed robotically. No mortality was recorded. Fifty-eight patients underwent total fundoplication, 1 patient had Collis-Nissen, 11 patients underwent partial fundoplication. Two gastric perforations were experienced and repaired robotically. Mean hospital stay was 38 hours (24-96). All patients were discharged on full liquid diet. Eight patients experienced dysphagia which eventually resolved within 4 weeks. Six patients (8.5%) recurred. Four were symptomatic and they underwent robotic REDO fundoplication and gastropexy, with three conversions to open approach. The use of the biosynthetic mesh made the REDO fundoplication very challenging, but doable. Two asymptomatic patients, discovered by upper gastrointestinal series at 3 months and 1 year, are on proton pump inhibitor therapy. No mesh complications were observed at median clinical follow-up of 27 months (6-49). Conclusions. Robotic fundoplication with biosynthetic mesh reinforcement provides a successful methodology in treating large paraesophageal hiatal hernias. Based on the low rate of recurrence of hiatal hernia, we speculate that the use of biosynthetic mesh leads to excellent clinical outcome in our patients. In recurred patients, the use of biosynthetic mesh creates a challenging REDO fundoplication. The high dexterity of robotic surgery helps to replicate the minimally invasive principles in the fundoplication technique, achieving the best outcome for our patients.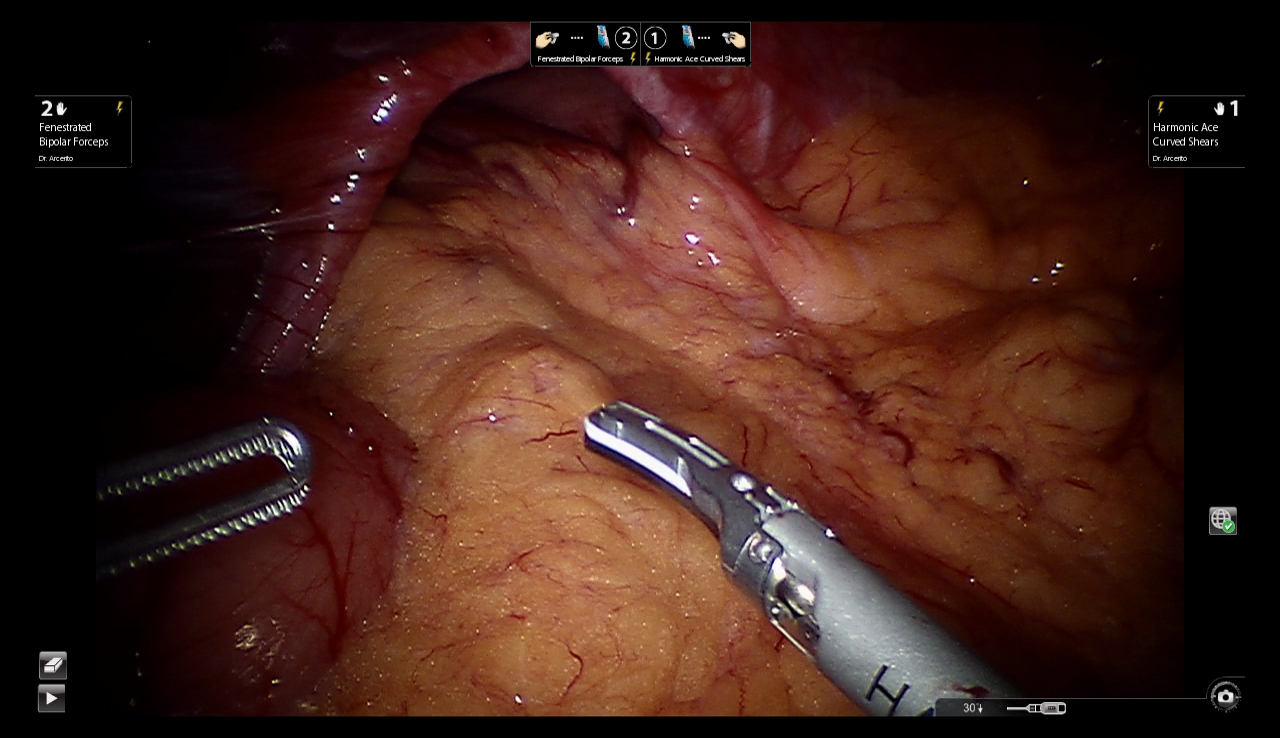
Paraesophageal hernia with large hiatus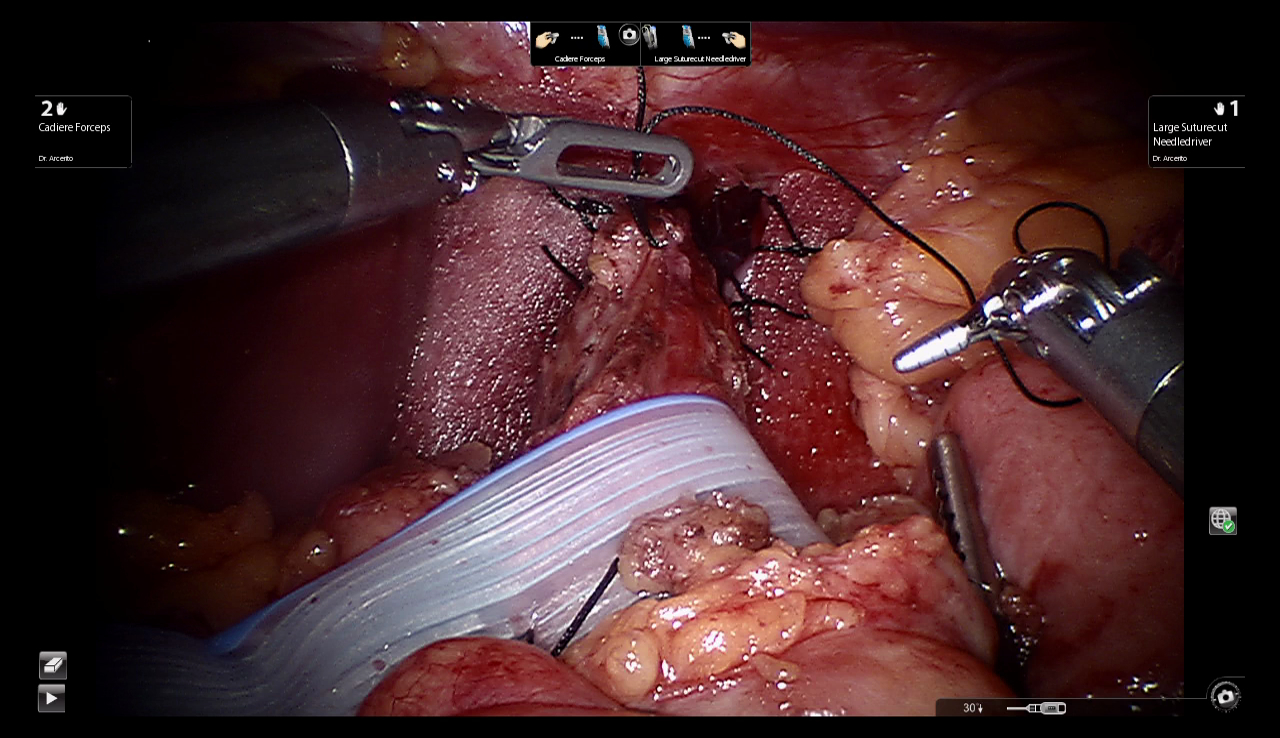
Biosynthetic Tissue Reinforcement Mesh
Back to 2019 Posters




