LAPAROSCOPIC AND ROBOTIC ASSISTED REPAIR OF GIANT PARAESOPHAGEAL HERNIAS ASSOCIATED TO PREVIOUS NISSEN FUNDOPLICATION: REPORT OF 38 CASES. TECHNICAL CONSIDERATIONS AND SURGICAL KEY POINTS.
Manuel P. Aguirre*, Javier A. Kuri, Francisco I. Galeana, Juan J. Solorzano
Surgery, American British Cowdray Hospital, Mexico, Mexico, Mexico
A giant paraesophageal hernia (PEH) is a complex surgical challenge that puts to the test the most experienced laparoscopic surgeons. Since the beginning of the laparoscopic era, it's getting more common to have patients with this type of hernias associated to a previous anti reflux surgery, making repair even more difficult to perform. When symptomatic, a paraesophageal hernia always needs surgical treatment, and the challenge depends directly on the size of the hernia, time since onset and its contents. The surgical technique for the repair of giant PEH's has evolved from the open abdominal, thoracic or combined procedures to the laparoscopic approach which has been the most accepted during the last 15 years, and nowadays, the robotic assisted approach. In this report, we intend to describe the technical considerations and surgical key points that will help laparoscopic and robotic surgeons to perform an adequate procedure ensuring the best possible outcome for their patients. Besides the advanced technical skills that every surgeon needs to deal with this complex hernia, the fact that most of the patients are above 60 years of age and with comorbidities, requires a multidisciplinary team to decide which patient will benefit from a surgical procedure.
38 patients with giant paraesophageal hernia where enrolled in this study. 21(55%) where treated by simple laparoscopic approach and 17 (45%) robotic assisted. Inclusion criteria included previous antireflux surgical procedure, giant paraesophageal hernia (≥10cm), an adequacy for surgical treatment. Mean surgical time for laparoscopic approach was 92 minutes (±27) and 127 (±22) for the robotic assisted. 10 surgical key points were established as essentials to obtain proper reduction, fixation and long-term results.
1.Reduce most of the hernia contents into the abdominal cavity. 2.The entire dissection of the hernia sac is imperative. 3.Always maintain crural integrity. 4.Always recover normal anatomy (undo 100% the previous fundoplication. Identify and pre-serve the anterior and posterior vagus nerve. 5.When planning an antireflux procedure (Nissen fundoplication) short gastric vessel dissection is always performed. 6.Always obtain the adequate esophageal length. 7.Avoid tension in crural closure. 8. Use biological mesh material to buttress the hiatal closure. 9.Be sure to create a fundoplication using the gastric fundus and not the body of the stomach. 10.Anterolateral gastropexy to abdominal wall is an excellent resource to prevent recurrence.
The laparoscopic repair of giant paraesophageal hernias represent a great challenge to the most experienced laparoscopic and robotic surgeons, that is why we intended to provide a list of clear steps that if followed correctly can make this procedure safe and effective, with low morbidity and mortality.
Giant paraoesophageal hernia.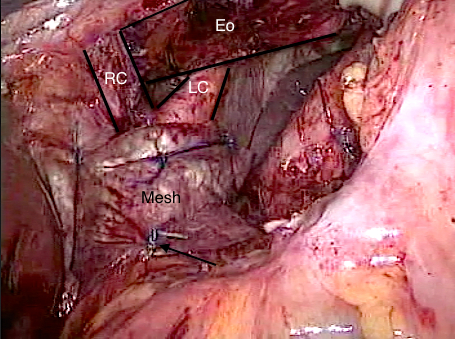
Crural closure and use of biological mesh.
Back to 2019 Posters




