SPLENIC INJURY MANAGEMENT - THE WAY FORWARD
Hannah S. Jesani*, Lara K. Jesani, Ashraf Rasheed
General Surgery, Royal Gwent Hospital, Newport, United Kingdom
Background
Splenic trauma is a life-threatening injury and cross sectional imaging is the most accurate diagnostic and grading investigation. Timely resuscitative laparotomy +/- total splenectomy is a life saving intervention in the presence of haemodynamic instability. In haemodynamically stable patients, selective non-operative management (SNOM) is a safe therapeutic strategy.1 The 1994 revised American Association for the Surgery of Trauma (AAST) severity grading of splenic injury is a useful tool guiding therapy especially in SNOM.2 The Baltimore CT Severity Index integrated splenic vascular injury to enhance the ability to support clinical decision making.3 Current evidence supports safety of SNOM in AAST grades I-III.4,5
Aim
To audit management of traumatic splenic injury over 15 years within a district general hospital, and CT reporting of AAST grading of splenic injury. By looking at current evidence we aimed to design a diagnostic and management pathway for patients admitted with splenic trauma.
Method
A retrospective database was established to capture all cases of splenic injury over 15 years from June 2002 to June 2017. The database was populated with demographics, CT AAST grading of splenic injury at presentation, management, and outcomes by reviewing clinical notes and electronic records. We captured all CT reports mentioning splenic injury during this period by searching an electronic database for the phrases "spleen injury/ laceration/ haematoma +/- trauma"?. We interrogated theatre records for operative cases coded as emergency splenectomy and cross-referenced this with histology.
Results
One hundred and thirty two (132) patients presented with splenic injury with M:F ratio 3:1. RTA was the most common mechanism of injury (35%). 57/132 (43%) patients were managed operatively and SNOM was undertaken in 75/132 (57%). Five patients (4%) had splenic artery embolisation while two (2) had operative splenorrhaphy and 56 underwent total splenectomy. 121/132 (92%) patients had CT imaging on admission but AAST grading was reported in 18/121 (15%) only. Comparing the first 7.5 years with the later 7.5 years, AAST grade reporting increased from 2/32 (6%) to 16/89 (18%) but this remains unacceptable. The use of SNOM increased significantly within our cohort over the studied period from 14/34 (41%) Vs. to 61/98 (62%); (p = 0.03). Overall mortality rate was 11.3%.
Conclusion
AAST grading of splenic injury remained sub-optimal over 15 years. There has been a significant move towards SNOM over this study period. The paradigm shift is probably multifactorial i.e. wider availability of multi-phase imaging to improve splenic injury characterisation, availability of splenic artery embolisation and advanced intensive care life support. An integrated multi-disciplinary diagnostic and management pathway might be the best way to reduce unnecessary splenectomy.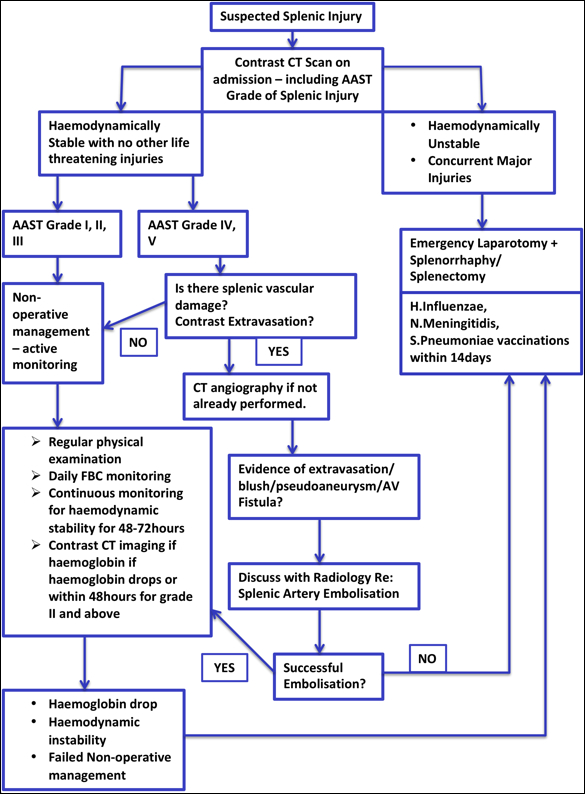
Suggested diagnostic and managment pathway for splenic injury
Back to 2019 Posters




