"A STITCH IN TIME"?: ADVANTAGES OF A HANDSEWN ILEOCOLIC ANASTOMOSIS IN COMPLICATED PATIENTS WITH CROHN'S ILEITIS
Mariane Camargo*1, Stephen Brandstetter1, Alexandra Aiello2, Luca Stocchi1, James M. Church1, Tracy L. Hull1, Ian Lavery1, Scott Steele1, Michael Valente1, Stefan D. Holubar1
1Colorectal Surgery, Cleveland Clinic Foundation, South Euclid, OH; 2Quantitative Health Sciences - Learner Institute, Cleveland Clinic Foundation, Cleveland, OH
Background
Ileocolic resection (ICR) is the most common surgical procedure for Crohn's disease (CD). Reconstruction is most commonly achieved with stapled side-to-side (SSTS) or hand-sewn (HS) ileocolic anastomosis (ICA), with the decision often made by tissue quality, surgeon experience and surgeon preference.We aimed to compare short-term complications and long-term recurrence-free survival of CD between patients who underwent SSTS vs. HS anastomoses in our institution.
Methods
This study was a retrospective analysis of a prospectively maintained database over a 5-year period. All patients who underwent ICR and ICA for terminal ileal CD from 01/2012-12/2016 were included. HS group included 53 end-to-end, 5 side-to-side, and 1 end-to-side cases. Patients who had a stoma, or other types of anastomoses, were excluded. The two groups were compared in a univariate analysis, and recurrence rates were assessed using Kaplan-Meier curves and a log-rank test. Cox-proportional hazard and linear regression models with propensity score inverse probability of treatment weighting were used to further evaluate postoperative outcomes and recurrence of CD. Numbers represent median or proportion as noted.
Results
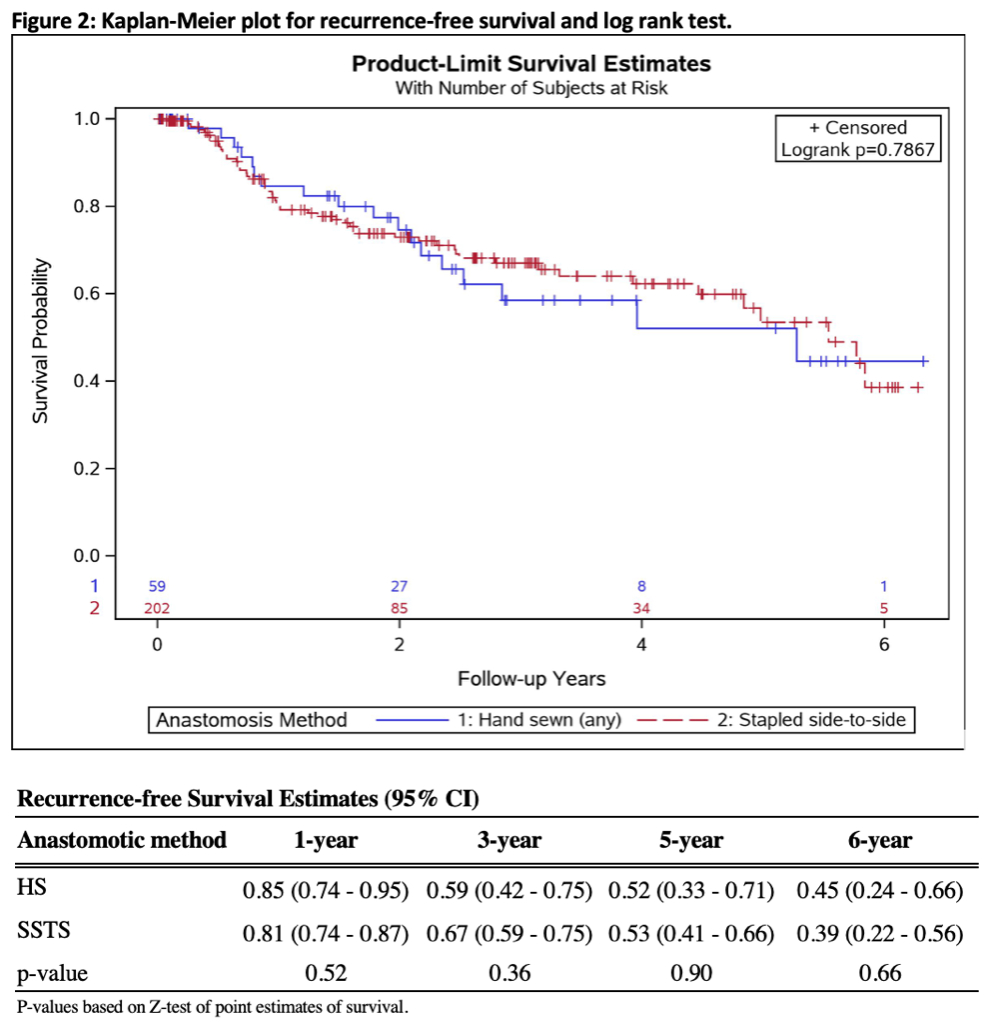
261 patients were analyzed: 59 in the HS group and 202 in the SSTS group. Patients in the HS group had a longer course of disease (16 vs. 9 years, p=0.005), were more likely to have previous surgeries (59% vs. 42%, p=0.02), perianal disease (39% vs. 23%, p=0.02) and redo ICA (56% vs. 33%, p=0.001). There was no difference between the groups in preoperative or postoperative use of medications. More HS patients were ASA class 3 (65% vs. 40%, p=0.004), and HS operations were longer (157 vs. 133min., p<0.001), with more blood loss (150 vs. 50ml, p<0.001), and fewer were laparoscopic (41% vs. 65%, p<0.001). Patients who underwent HS compared to STSS had surgeons with more years of experience, 16 vs. 11 years, p<0.001, respectively. For postoperative outcomes, HS patients had longer lengths of stay (6 vs. 5 days, p=0.02).The Kaplan-Meier analysis for recurrence showed no difference in recurrence rates. After propensity score weighting and adjustment for covariates, HS patients had less than 1/3 of the odds of major (Clavien-Dindo ≥3) complication compared to the SSTS group (OR0.29 [0.09 - 0.92], p=0.035).
Conclusion
At our center after ICR for CD, HS anastomoses, compared to SSTS anastomoses, were observed to be independently associated with a lower rate of major postoperative complications, despite being significantly more complex patients. However, no difference in recurrence rates between the HS and SSTS anastomoses was observed. Thus, colorectal surgeons should be facile and confident in performing HS procedures, especially in difficult situations (advanced and recurrent disease, previous surgeries, and high morbidity patients), lest HS become a lost art.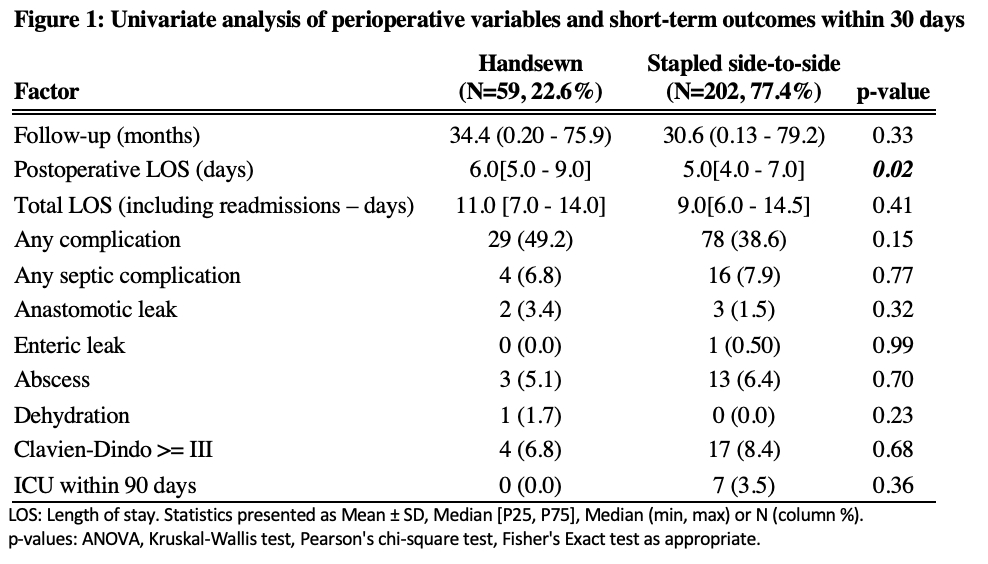
Back to 2019 Posters




