PREDICTORS OF POST-DISCHARGE MORTALITY IN ELECTIVE COLECTOMY
Carl Johnson*, Lauren Wood, Joshua Richman, Amandiy Liwo, Frank Gleason, Melanie Morris, Daniel I. Chu, Jamie A. Cannon, Gregory D. Kennedy
University of Alabama at Birmingham, Birmingham, AL
Objective: Patients that have post-operative complications are at increased risk for mortality and likely require close follow-up. We sought to identify factors that could predict mortality in patients following major in-hospital complications that have undergone a colectomy.
Methods: Colectomies requiring an anastomosis were acquired from the 2005-2017 American College of Surgeons National Surgical Quality Improvement Program participant use files. Emergent colectomies were excluded from this analysis. We identified patients who were discharged alive and who had at least one major complication prior to discharge. Major complications included: sepsis, septic shock, pneumonia, deep vein thrombosis, pulmonary embolism, myocardial infarction, reintubation, stroke with neurological deficit, and cardiac arrest requiring CPR. Log rank tests and adjusted cox regression models were used to identify independent risk factors for post-discharge mortality.
Results: There were a total of 281,676 patients in this cohort with an overall mortality rate of 0.43%. 14,624 patients experienced a complication and the mortality rate for this group was significantly increased compared to the overall cohort (2.07%; p < 0.001). Age, partial or total dependent functional status, stroke, pneumonia, reintubation, and septic shock were all independent risk factors for post-discharge mortality. Elective surgery and longer hospital length of stay following last complication were associated with a lower risk of post-discharge mortality. The complete cox regression analysis is shown in Table 1.
Conclusions: Patients that had major in-hospital complications were at almost five times the risk of dying after a colectomy. These patients may benefit from a longer hospital stay following their complication and may warrant modified outpatient surveillance to improve mortality rates.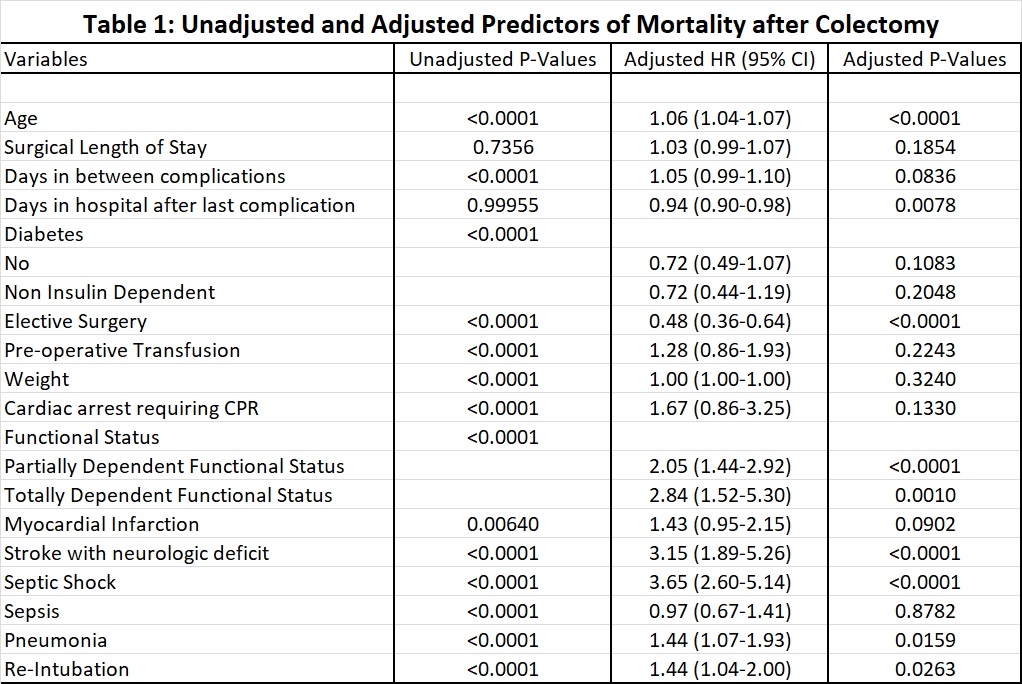
Back to 2019 Posters




