OPTIMAL MANAGEMENT OF MUCINOUS RECTAL CANCER: A STUDY OF THE NATIONAL CANCER DATABASE
Beiqun Zhao*, Samuel Eisenstein, Lisa A. Parry, Benjamin Abbadessa, Bard C. Cosman, Sonia Ramamoorthy, Nicole E. Lopez
Surgery, University of California, San Diego, La Jolla, CA
Introduction:
Mucinous rectal adenocarcinoma (MRA) is a distinct clinical subtype of rectal cancer. It occurs far less frequently than non-mucinous rectal adenocarcinoma and is generally associated with poorer outcomes. It is commonly accepted that MRA is relatively resistant to both chemotherapy and radiotherapy. However, few studies have examined optimal treatment strategies for patients with MRA and it is frequently treated in a similar fashion to non-mucinous rectal adenocarcinoma. In this study, we aim to determine best management strategies for patients presenting with clinically defined stage II and III MRA.
Methods:
The National Cancer Database (NCDB) was used to identify patients with histology confirmed stage II or III MRA between 2004 and 2015. Overall survival (OS) by treatment modality was compared using Kaplan-Meier analysis. Predictors for OS in patients who underwent surgery were analyzed using univariable and multivariable Cox regression modeling.
Results:
A total of 4,278 patients were identified and included in the analysis. Patients presented at a median age of 62 years (range 18-90). Patients were predominantly male (72.8%) and white (84.5%). Patients most commonly presented with stage IIA (38.2%) and IIIB (36.4%) disease. Most tumors were well- or moderately-differentiated (75.5%), T3 (77.6%), and N0 or N1 (47.8% and 40.8%, respectively). Most patients were treated with radiation (85.1%) and chemotherapy (89.0%). The median OS of patients who had surgery alone (38.5 months, 95% CI 33.4 - 43.6) was shorter than surgery + radiation therapy (56.1 months, 95% CI 30.1 - 82.0), surgery + chemotherapy (64.6 months, 95% CI 40.9 - 88.3), and surgery + radiation + chemotherapy (96.8 months, 95% CI 87.1 - 106.5). On multivariable Cox analysis (Table 1), increasing age, increasing Charlson-Deyo comorbidity score, high-risk tumor grade, cT4 tumors, and higher cN stages were associated with decreased OS. Negative margins (HR 0.56, 95% CI 0.48-0.65, p<0.001) and chemotherapy (HR 0.58, 95% CI 0.46 - 0.73, p<0.001) were associated with improved OS. Radiation therapy was not a significant predictor of OS.
Conclusion:
This study demonstrates the importance of achieving negative resection margins and using multimodal therapy consisting of chemotherapy in combination with surgery in order to achieve maximal survival in patients with MRA. While there was no observed survival benefit from radiation, potential advantages of radiation, such as its effect on margin negative resection and local recurrence, are not well assessed by data included in the NCDB. Future studies are necessary to further clarify the role for radiation in the treatment of MRA.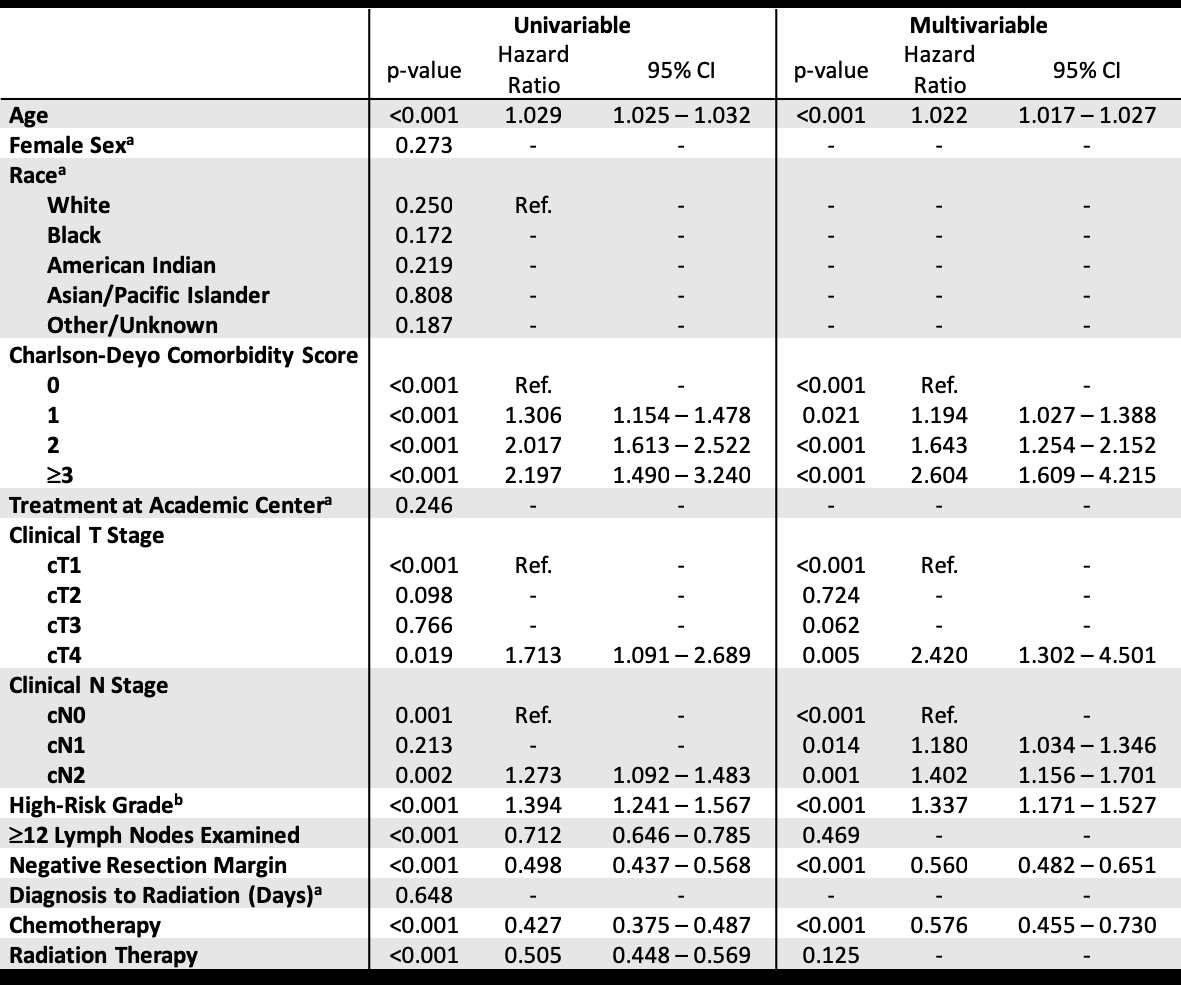
Table 1. Univariable and multivariable Cox regression analysis for predictors of overall survival in patients with MRA.
aCriteria for entry into multivariable model set at p<0.20
bHigh-risk grade = poorly differentiated, undifferentiated, or anaplastic tumor grade
Back to 2019 Posters




