PREDICTORS OF COMPLICATIONS FROM STOMA CREATION IN ELECTIVE COLORECTAL SURGERY: AN ASSESSMENT FROM THE AMERICAN COLLEGE OF SURGEONS NATIONAL SURGICAL QUALITY IMPROVEMENT PROGRAM (ACS NSQIP)
Thais Reif de Paula*1, Samantha K. Nemeth2, James M. Kiely1, Deborah S. Keller1, Ravi P. Kiran1,2
1Surgery, Division of Colorectal Surgery, Columbia University Medical Center, New York, NY; 2Center for Innovation and Outcomes Research, Columbia University Medical Center, New York, NY
Background: A diverting loop ileostomy (DLI) can be used to protect a high risk or distal colorectal anastomosis, particularly after low anterior resection or restorative proctocolectomy. While a DLI serves a functional purpose, complications after an ileostomy are common and can be costly. These complications may impact on quality of life, require readmissions, further surgery, and contribute to mortality and healthcare costs. The burden of stoma related morbidity for patients is therefore significant, and identifying predictors of complications could serve great benefit for patients and providers. Our goal is to define the incidence and risk factors of postoperative morbidity after the creation of elective DLI.
Methods: From the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) colectomy targeted data, patients who underwent elective DLI creation as part of a major abdominal colorectal procedure from 2012-2016 were identified by Current Procedural Terminology procedure codes. Demographic and clinical characteristics, operative, and postoperative outcomes were evaluated. The primary outcome measures were 30-day major morbidity (Clavien class III and greater), surgical site infections (SSI), ileus, and readmission rates. Multivariate logistic regression models were created to assess the risk factors associated with these outcomes.
Results: 5,026 patients were evaluated. The sample had a median age of 59 [IQR 50-67] years, median body mass index (BMI) 27.44 [IQR 23.96-31.63] kg/m2 and was 56.2% male. The median operative time was 257 [IQR 192-371] min, and median total LOS was 6 [IQR 4-8] days. 38.2% experienced major morbidity, including SSIs (11.7% overall, 5.1% superficial, 1.1% deep, 6.1% organ space), sepsis (3.4%), urinary tract infection (3.0%), septic shock (1.2%), and pneumonia (1.3%). 18.1% were readmitted, and 4.7% required reoperation. On multivariate logistic regression, male gender, operative time, and an open approach (vs. laparoscopic) were some of the risk factors associated with increased odds of major morbidity (See Table 1). White cell count (WCC), disseminated cancer, and operative time were independent risk factors for overall SSI. Diabetes and hypertension were associated with increased odds of readmission. Male gender, disseminated cancer, and Wound Class 3 were associated with increased odds of ileus.
Conclusions- While DLI creation is performed to reduce complications, there are major complications associated with the procedure itself. From the analysis, modifiable factors were found to be associated with postoperative outcomes after DLI creation. Using these results can help prospectively prepare for these high-risk patients, potentially improving postoperative outcomes and surgical quality with DLI creation.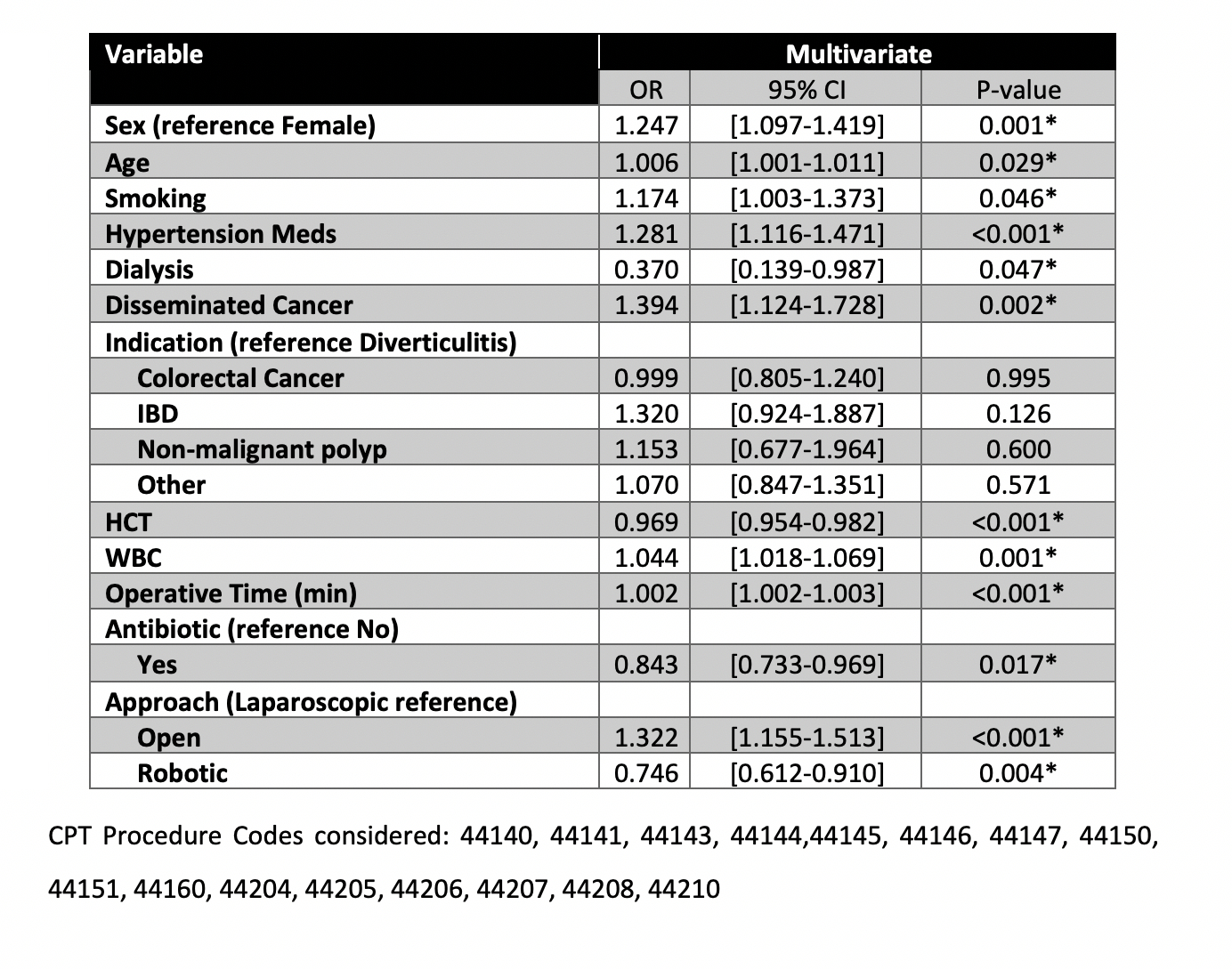
Back to 2019 Posters




