SCREENING FOR COLORECTAL CANCER: WHEN SHOULD WE START? WHEN SHOULD WE STOP? AN ANALYSIS OF CASES FROM THE SEER PROGRAM
Luv Hajirawala*1, Carla B. Rosales2, Guy R. Orangio1, Jeffrey Barton1, Kurt Davis1
1General Surgery, LSU Health Sciences, New Orleans, LA; 2Louisiana Tumor Registry, New Orleans, LA
Background
The age to begin and cease screening for colorectal cancer (CRC) is debated. The United States Preventative Services Task Force guidelines (USPSTF) recommend that patients between the ages of 50 and 75 obtain screening for CRC. This study aims to review the CRC stages at diagnosis for patients within the current 50-75-year age range and compare them to those patients who are either younger than or older than the recommended screening ages.
Methods
CRC cases diagnosed between 2011 and 2015, collected by the Surveillance, Epidemiology, and End Results (SEER) program of the National Cancer Institute were included in the analysis. Patients with Stage I and II CRC were considered early stage, and Stage III and IV patients were considered as late stage for comparison. The patients were stratified into those within the current screening guidelines (ages 50-74), and patients younger (ages 45-49) or older (ages 75+) than the USPSTF guidelines. The incidence rates of early and late stage CRC were compared among the age groups. Yearly trends in the rate of CRC among the age groups were also evaluated.
Results
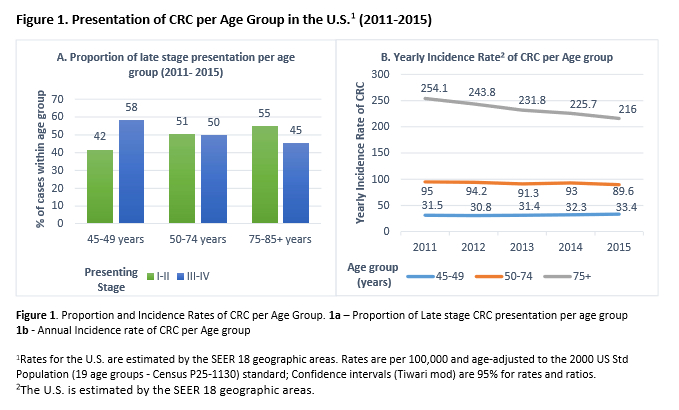
A total of 156,084 patients with CRC between 2011 and 2015 were included in the analysis. Overall, 49% of patients presented with late stage disease. For the younger group, 58% presented with Stage III or IV CRC, compared to 50% in the screening age range and 45% the older group (Figure 1a). The incidence rate of late stage CRC was significantly higher than that of early stage CRC in the younger age cohort (Table 1).
Patients older than the currently screened cohort account for 33.3% (51,990) of CRC cases (Table 1). The rate of CRC is highest in this group, followed by patients in the screening age cohort, with the lowest in the younger group (Figure 1b). While the rate of CRC is on the decline in both the older than screening age and current screening age populations, the rate of CRC in younger (ages 45-49) patients does not demonstrate a decrease (Figure 1b).
Conclusions
Patients who are not screened tend to present at the onset of symptoms from CRC, such as bleeding or obstruction, which often corresponds to later stage at presentation. The rate of advanced CRC in the younger population remains stable through the studied period, in contrast to the declining rates seen in the other two study populations. Screening appears to accomplish the goal of identification of earlier stage cancer, which argues for lowering the screening age for CRC.
Since a significant percent of CRC presents in patients older than the current screening window, and the majority are treated surgically, expanding screening guidelines to these patients as well appears justified. Expanding the age limits for screening for CRC should help capture patients at an earlier stage, thus improving their overall prognosis and survival.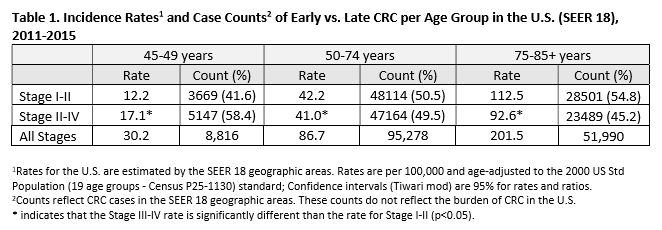
Back to 2019 Posters




