LAPAROSCOPIC BOTULINUM TOXIN PYLOROPLASTY IS SAFE AND MAY IMPROVE POST-OPERATIVE OUTCOMES AFTER SLEEVE GASTRECTOMY
Robinson Tyler*, Vladimir Davidyuk, Sara Khan, Vanbacker Justin, ashar ata, Tejinder Singh, Jessica Zaman
Surgery, Albany Medical College, Albany, NY
Background: Chemical pyloroplasty using botulinum toxin has been shown to provide effective surgical drainage after esophagectomy, reducing postoperative complications and improving the peri-operative patient experience. We suggest that botulinum toxin pyloroplasty (BP) during laparoscopic sleeve gastrectomy (SG) can reduce gastric pressure, improve gastric emptying post-operatively, reduce post-operative nausea and vomiting, and enhance recovery after surgery. This retrospective analysis demonstrates the safety and efficacy of BP, which has been performed in conjunction with SG at our institution since 2010.
Methods: We conducted a retrospective chart review of patients undergoing laparoscopic or robotic-assisted SG by three surgeons at our institution over a five-year time period. BP was performed laparoscopically by administering 100 U of botulinum toxin suspended in 10 mL of saline into the pylorus using a spinal needle after completion of stapling during SG. Patient demographics, operative variables, and 30-day post-operative outcomes were extracted from electronic medical records. The Clavien-Dindo Classification system was used to compare the severity of postoperative complications of patients in both cohorts.
Results: Of the 589 patients undergoing SG from 2010-2015, 469 patients received BP and 120 patients did not. There were no statistically significant differences in age, gender, pre-operative BMI, or obesity- related co-morbidities between the two cohorts. There no statistically significant differences in overall complications between the BP and the no-BP group (4.5% vs 2.5%, OR 1.79, CI 0.5-9.5). The average Clavien-Dindo score was 2.0 for the BP group, and 2.3 for the no-BP group. The most common complication for the BP group was dehydration requiring admission or outpatient hydration (n = 8). The only leak occurred in the no-BP group. The average hospital length of stay was 3 for the BP group, compared to 3.45 for the no-BP group.
Conclusions: Botulinum toxin pyloroplasty following sleeve gastrectomy does not increase the rate or severity of postoperative complications after SG. Preliminary evidence demonstrates that BP may reduce post-operative nausea and vomiting, improve length of stay, and reduce the incidence of leaks. A randomized controlled trial to assess the benefit of chemical pyloroplasty in conjunction with traditional enhanced recovery after surgery measures is ongoing at our institution.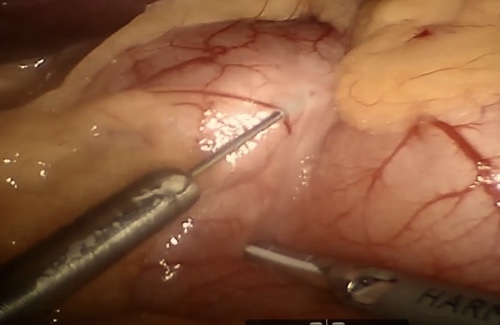
Laparoscopic injection of 100 U botulinum toxin into the pylorus using a spinal needle.
Back to 2019 Posters




