PANCREATIC DUCT CALIBER DOES NOT RELIABLY DISTINGUISH MALIGNANT FROM PREMALIGNANT MAIN DUCT IPMNS
Tara Hughes*1, Laura R. Prakash1, Anirban Maitra2, Manoop S. Bhutani3, Florencia McAllister4, William A. Ross3, Brian R. Weston3, Eugene Koay5, Huamin Wang2, Jeffrey Lee3, Jean-Nicolas Vauthey1, Jeffrey E. Lee1, Thomas Aloia1, Ching-Wei Tzeng1, Matthew Katz1, Michael P. Kim1
1Surgical Oncology, MD Anderson Cancer Center, Houston, TX; 2Pathology, MD Anderson Cancer Center, Houston, TX; 3Gastroenterology, MD Anderson Cancer Center, Houston, TX; 4Clinical Cancer Prevention, MD Anderson Cancer Center, Houston, TX; 5Radiology, MD Anderson Cancer Center, Houston, TX
Background: Main duct intraductal papillary mucinous neoplasms (MD-IPMN) are at significant risk for progression into pancreatic ductal adenocarcinoma (PDAC). Previous studies indicate the risk for malignant transformation proportionally increases with the caliber of MD-IPMNs, approaching a >50% incidence of PDAC in MD-IPMNs ≥1cm. For this reason, current guidelines recommend MD-IPMNs with calibers ≥1cm undergo surgical resection. We sought to determine the validity of this recommendation based on our experience at a high-volume, academic center.
Methods: Review of a prospectively maintained, retrospective database identified 71 patients who underwent pancreatic resection for MD-IPMN from 2005-2018. Preoperative MD-IPMN calibers were individually measured on CT or MRI imaging and preoperative CA 19-9 values and radiographic imaging characteristics were recorded for each patient. Patients with MD-IPMNs were grouped based on the presence of LGD/MGD, HGD or PDAC on final pathologic analysis. Student's t-tests were used to test differences in duct caliber and CA 19-9 values between patient subgroups and the sensitivities and specificities were calculated for preoperative nodularity/masses to represent PDAC.
Results: Among 71 patients with MD-IPMNs, final pathology revealed LGD/MGD in 13, HGD in 26 and PDAC in 32. Duct caliber was not significantly different between MD-IPMNs with LGD/MGD and HGD (12 ±5.2 mm vs. 14 ±7.8 mm, respectively; p=0.44). Moreover, no significant differences were identified in the calibers of MD-IPMNs harboring LGD/MGD or HGD relative to PDAC (12.6 ±6.5 mm; p=0.91 & p=0.38). CA 19-9 levels were not significantly different between MD-IPMNs with LGD/MGD and HGD (23.8 ±19.8 U/ml vs. 25.8 ±31.9 U/ml, respectively; p=0.84) and approached significance between MD-IPMNs with LGD/MGD and PDAC (23.8 ±19.8 U/ml vs. 87.3 ±112 U/ml, respectively; p=0.05). A solid nodule or mass was observed on preoperative EUS, CT or MRI in 6/13 patients with LGD/MGD, 16/26 with HGD and 30/32 with PDAC. Collectively, the presence of preoperative nodules/masses had a sensitivity of 93.75% (95% CI 79.2-99.2) and specificity of 43.6% (95% CI 27.8-60.4) for PDAC.
Conclusion: Neither pancreatic duct diameter ≥1 cm nor elevations in CA19-9 levels consistently correlate with the underlying presence of PDAC in association with MD-IPMNs. Nodularity or masses associated with MD-IPMNs on preoperative imaging were sensitive for the presence of PDAC but inadequate to distinguish premalignant lesions from PDAC. In the absence of biopsy-proven HGD/PDAC, MD-IPMN calibers ≥1cm should not solely be used to justify surgical resection, particularly in high surgical risk patients. MD-IPMN duct caliber should be considered with other high-risk stigmata and/or worrisome features to inform decisions regarding resection of MD-IPMNs.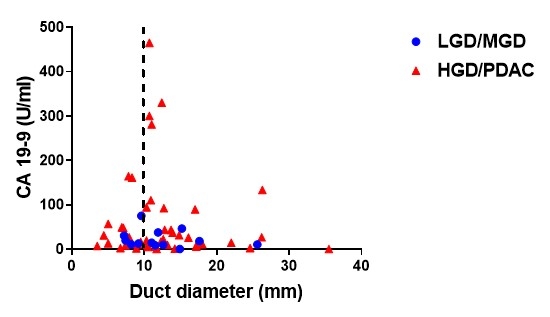
Back to 2019 Posters




