PSEUDOACHALASIA FOLLOWING MAGNETIC SPHINCTER AUGMENTATION WITH RECOVERY OF PERISTALSIS FOLLOWING DILATION: A CASE REPORT
Shahin Ayazi, Madison Salvitti*, Toshitaka Hoppo, Michelle Gonzalez, Ali H. Zaidi, Blair A. Jobe
Esophageal and Lung Institute, Allegheny Health Network, Pittsburgh, PA
Introduction:
Pseudoachalasia is mimicking clinical and physiologic manifestations of idiopathic achalasia but results from alternative etiology for outflow obstruction at the gastroesophageal junction (GEJ).
We report a case of pseudoachalasia that occurred 14 months after magnetic sphincter augmentation (MSA) and resolved with endoscopic dilation.
Case presentation:
In this case, we present a 54-year-old man with longstanding gastroesophageal reflux disease (GERD). His primary symptom of heartburn was proton pump inhibitor (PPI) responsive and he denied any preoperative dysphagia. He underwent complete preoperative foregut evaluation. A Bravo pH monitoring showed abnormal DeMeester scores of 28.3 and 24.5 for days 1 and 2. His high-resolution manometry (HRM) showed peristaltic progression of esophageal body contractions in all swallows with normal mean amplitude and normal distal contractile integral (DCI), and a normotenisve LES with partial relaxation. His videoesophagram showed a 1cm small hiatal hernia and no evidence of esophageal dysmotility.
He underwent hiatal hernia repair and magnetic sphincter augmentation using a size 15 LINX device. The surgery was uneventful, and he was discharged on the same day. Few days after surgery, he was complaining of chest pain and dysphagia, these symptoms were completely resolved with adherence to post-LINX diet consisted of frequent small meals and a short course of steroid. Fourteen months after surgery, he presented to our clinic with complaint of progressive dysphagia, this prompted a foregut objective evaluation that showed normalization of distal esophageal acid exposure. His HRM showed complete aperistalsis in the esophageal body and 0% bolus clearance on impedance analysis and a non-relaxing LES with elevated integrated relaxation pressure (IRP) of 21.2 mmHg. Videoesophagram showed a poor relaxation of the GEJ with hold up of the liquid barium contrast above the GEJ. Patient then underwent an EGD which showed a moderate degree of tightness at GEJ, which was dilated using 57 and 60 French savory dilators. He had partial relief of his dysphagia after this procedure. Eight weeks later, he underwent another EGD and dilation with 18-20 mmHg balloon with complete resolution of his dysphagia. A follow up HRM showed restoration of peristaltic esophageal contractions with normal mean amplitude and DCI and a completely relaxing LES with normalization of IRP and normal intrabolus pressure. Patient has remained free of symptom of dysphagia since then.
Conclusion:
Magnetic sphincter augmentation is increasing GEJ outflow resistance. This increase in the resistance, in this case led to outflow obstruction resulting aperistalsis and pseudoachalasia. Endoscopic dilation resolved the dysphagia and restored the peristaltic function of the esophagus (Figure).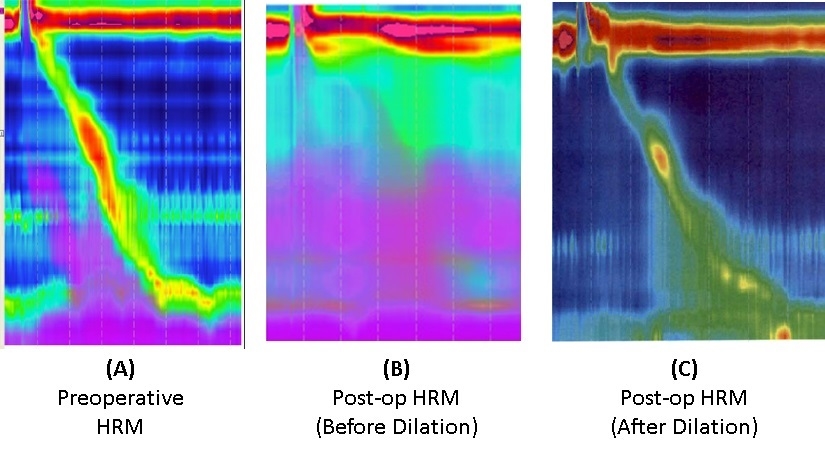
Back to 2019 Posters




