ANALYSIS OF COUNTY-LEVEL ACCESS TO SPECIALIZED PROVIDERS ON COLORECTAL CANCER INCIDENCE AND MORTALITY IN ILLINOIS
Jonathan R. Day*1, Vivek Prakash3, Whitney Zahnd2, Mustafaa Mahmood1, V. Prasad Poola1, Jan Rakinic1, Sabha Ganai1
1Department of Surgery, Southern Illinois University, Springfield, IL; 2University of South Carolina Arnold School of Public Health, Columbia, SC; 3Center for Clinical Research, Southern Illinois University, Springfield, IL
Introduction: Disparities in colorectal cancer (CRC) screening, incidence, and mortality include race/ethnicity, geographic proximity, insurance, and other socioeconomic factors. Studies have identified provider shortages in rural areas. Previous research has shown rural Illinoisans experience a higher travel time to fellowship-trained colorectal surgeons. We hypothesized that access to various CRC specialists would be associated with CRC outcomes.
Methods: Practice location data on IL colorectal surgeons (CRSurg), radiation oncologists (RadOnc), EUS-capable gastroenterologists (EUS-GI) were geocoded. Multiple linear regression (ordinary least squares) was used with number of providers of each type per 100,000 persons per county to assess the relationship to provider density on colorectal cancer incidence and mortality. The relationship of median age, race, insurance status, and socioeconomic status by income quartile to CRC incidence, and CRC mortality were investigated via multiple linear regression (ordinary least squares). Models were bootstrapped to account for counties with extreme mortality values.
Results: We found no significant relationship between county-level density of CRSurg (OR 0.58; 95% CI, 0.06 - 4.75), RadOnc (OR 1.39; 95% CI, 0.64 - 2.73) and EUS-GI (OR 0.41; 95% CI, 0.02 - 29.8) and CRC incidence after confounding control. We also found no significant relationship between access to CRSurg (OR 0.93; 95% CI, 0.32 - 1.92), RadOnc (OR 0.92; 95% CI, 0.75 - 1.36) and EUS-GI (OR 0.67; 95% CI, 0.15 - 3.14) and CRC mortality after confounding control. There was a significant relationship between highest income quartile and decreased CRC incidence and mortality across all provider models.
Conclusion: We were unable to find a difference in CRC incidence or mortality in the state of Illinois with regard to access to colorectal surgeons, radiation oncologists, and EUS-capable gastroenterologists. The data did suggest an important inverse relationship between highest income and CRC outcomes after confounding control across all models. This is consistent with national data demonstrating disparities in cancer mortality and across low-, medium-, and high-income counties. Further study will be needed to examine how CRC outcomes in Illinois can be influenced as well as follow up of the counties with highest mortality. 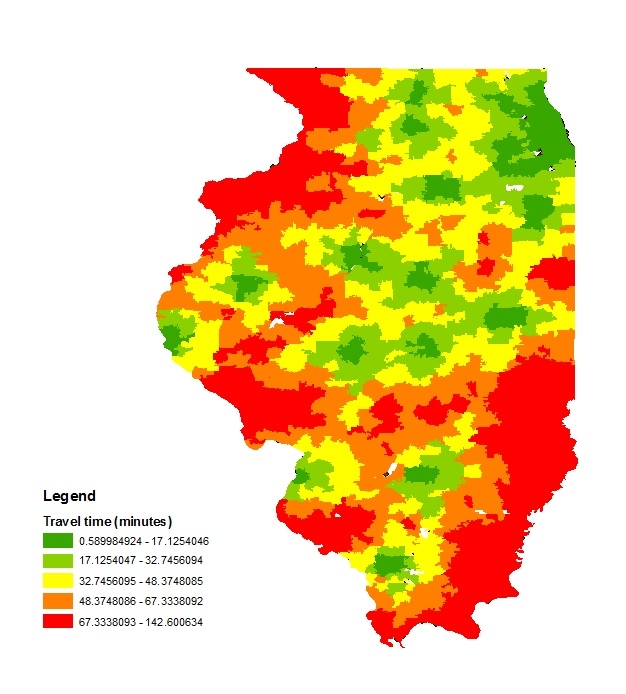
Choropleth map of accessibility by travel time to colorectal surgeons in Illinois.
Back to 2019 Posters




