RACIAL DIFFERENCES IN THE RECEIPT OF SURGERY FOR APPENDICITIS, CHOLECYSTITIS AND GALLSTONE PANCREATITIS
John Bliton*, Michael K. Parides, Flavio Malcher, Prashanth Sreeramoju, Haejin In
Montefiore Medical Center, Bronx, NY
Background
Appendicitis and cholecystitis are two of the most common indications for surgery in the United States. Timely resection of the diseased organ decreases risks of recurrence and morbidity as well as cost. However, literature suggests that racial disparities in receipt of surgery may exist. We aim to utilize a nationally representative sample of US hospital discharges to examine whether racial differences are present in receipt of surgery for these indications.
Methods
The National Inpatient Sample (NIS) was used to identify patients with discharge diagnoses of appendicitis, cholecystitis, and gallstone pancreatitis in years 2008-2012. Patient factors, hospital factors, and ED admission were examined for each racial group. Generalized linear mixed regression was used to evaluate the impact of race on receipt of surgery, controlling for other variables. A secondary analysis examined the impact of including other diagnosis-specific temporizing procedures: drainage of abscess or gallbladder via percutaneous catheterization, or biliary track clearance via endoscopic retrograde cholangiopancreatography (ERCP). The impact of receipt of surgery on racial differences in inpatient mortality was also examined. Analysis was conducted using SAS 9.4 (Cary, NC).
Results
233,567 patients with appendicitis, 282,854 patients with cholecystitis and 55,226 patients with gallstone pancreatitis were included in the study. Black patients had lower age-standardized operative rates compared to White patients; 92.2% vs 95.6%, 81.7% vs 87.1%, and 42.6% vs 48.4% for these diseases, respectively. Compared to White patients, Black patients were younger (mean age: 44.4 vs 49.1 years), had more comorbidities (1 or more: 44.6% vs 40.8%), came from lower-income ZIP codes (lowest quartile: 44.9% vs 20.7%), had higher rates of ED admission (82.6% vs 78.4%) and were less likely to have private insurance (35.0% vs 50.0%). On multivariate analysis, the adjusted odds ratios for receipt of surgery comparing Black to White patients were 0.70 (95% CI 0.65-0.76), 0.77 (95% CI 0.74-0.81) and 0.77 (95% CI 0.72-0.83) for appendicitis, cholecystitis and gallstone pancreatitis, respectively. The inclusion of temporizing measures did not greatly alter these results. Receipt of surgery did not contribute to differences in in-hospital mortality.
Conclusion
Black patients are less likely to receive surgery during an admission for appendicitis, cholecystitis and gallstone pancreatitis. While inequality in rates of surgery did not seem to explain the increased mortality observed for Blacks, it may contribute to racial disparities for other meaningful long-term outcomes, such as readmissions and complexity of future surgeries. Further study is needed to investigate the underlying causes of racial inequality in rates of surgery.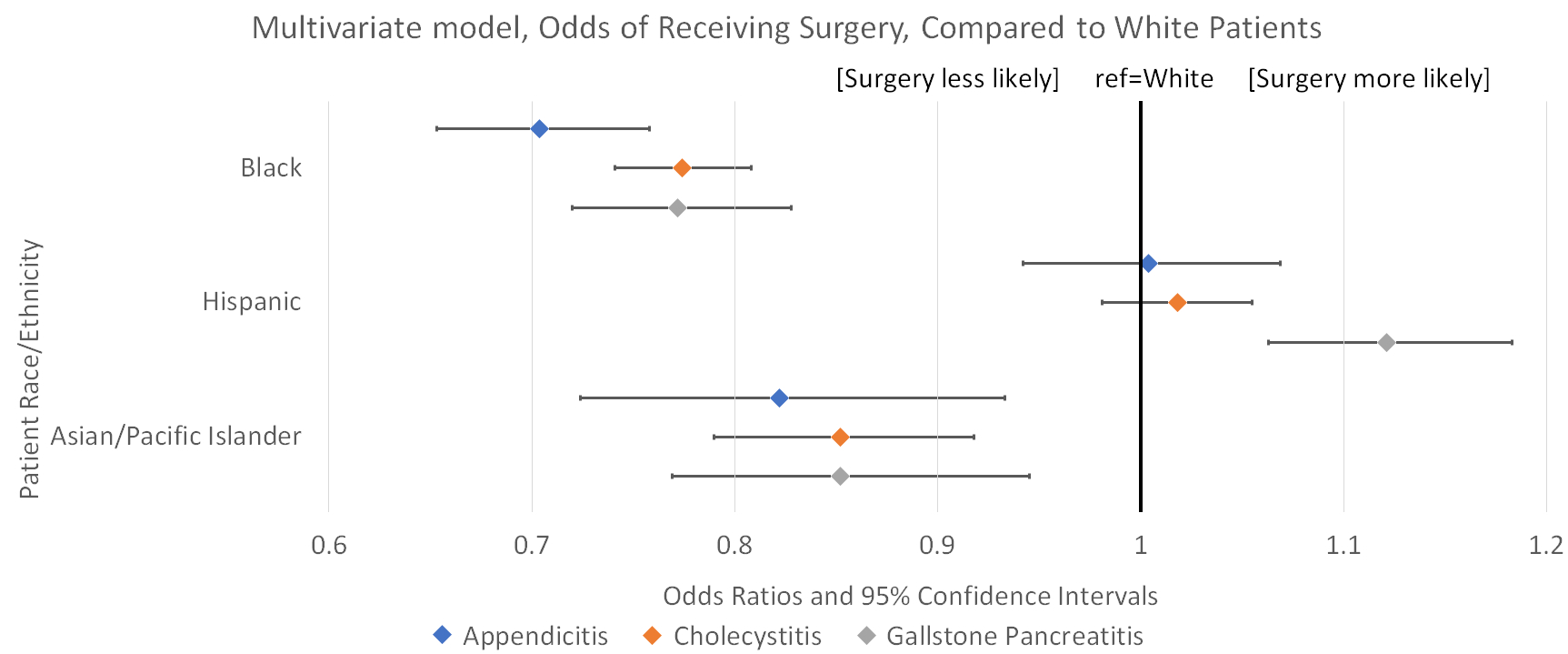
Back to 2019 Posters




