CLOSTRIDIUM DIFFICILE AFTER LAPAROSCOPIC BARIATRIC SURGERY: AN ANALYSIS OF THE METABOLIC AND BARIATRIC SURGERY ACCREDITATION AND QUALITY IMPROVEMENT PROGRAM
ThucNhi T. Dang*, Jerry Dang, Muhammad Moolla, Noah Switzer, Karen Madsen, Daniel W. Birch, Shahzeer Karmali
University of Alberta, Edmonton, AB, Canada
Background: Obesity is associated with disturbances in the gut microbiota and reduced microbial diversity, both of which are risk factors for Clostridium difficile infection (CDI). Patients undergoing bariatric surgery incur substantive changes to their gut microbiota which may affect their risk for developing CDI.
Aims: Assess the risk of developing postoperative CDI within 30 days after laparoscopic Roux-en-Y gastric bypass (LRYGB) and laparoscopic sleeve gastrectomy (LSG)
Methods: The Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) is a clinically-rich database that captures variables specific to bariatric surgery from 791 centers in the United States and Canada. We identified all patients undergoing LRYGB or LSG in 2016 and 2017. Patients undergoing revisional bariatric surgery were excluded. Primary outcomes of interest included the prevalence and predictors of CDI after bariatric surgery. A purposeful selection algorithm was used to develop a multivariable logistic regression model to determine preoperative factors predictive of 30-day CDI.
Results: A total of 78,222 LRYGB and 222,968 LSG were included. Mean age was 44.5 ± 12.0 years, 79.6% were female and mean body mass index was 45.3 ± 7.8 kg/m2. The overall incidence of CDI among patients undergoing LRYGB or LSG was low with only 383 patients (0.13%) developing CDI within 30-days post-bariatric surgery. Rates of CDI were two-times higher in the LRYGB cohort compared to the LSG cohort (0.2 vs 0.1%, p < 0.001).
Although incidence of CDI overall was low, CDI post-operatively was associated with increased length of stay (LOS) and surgical complications including anastomotic leaks, deep surgical site infection, re-operations, re-intervention, and re-admissions within 30 days. Additionally, it was associated with increased risk of other complications including pneumonia, acute kidney injury (AKI), VTE, sepsis, and unplanned intubation (Table 1). It was not, however, associated with increased risk of death.
Multivariable analysis identified CKD (OR 2.37 [CI 95% 1.09-5.15, p = 0.03]) and history of VTE (OR 2.06 [CI 95% 1.29-3.29, p = 0.002]) as being most predictive of developing CDI 30-day post-bariatric surgery with more than a two-fold increase in risk. Patients undergoing LRYGB had increased the risk of CDI post-surgically compared to LSG (OR 1.65 [CI 95% 1.31-2.09, p < 0.001]). White race, female sex, and obstructive sleep apnea (OSA) also increased risk of post-surgical CDI.
Conclusions: The incidence of CDI following bariatric surgery remains lower than both the inpatient medical and general surgery populations. LRYGB had a higher risk of CDI compared to LSG, although the exact mechanism is unknown. Furthermore, CDI is associated with significant adverse outcomes post-operatively but had no increased risk of mortality.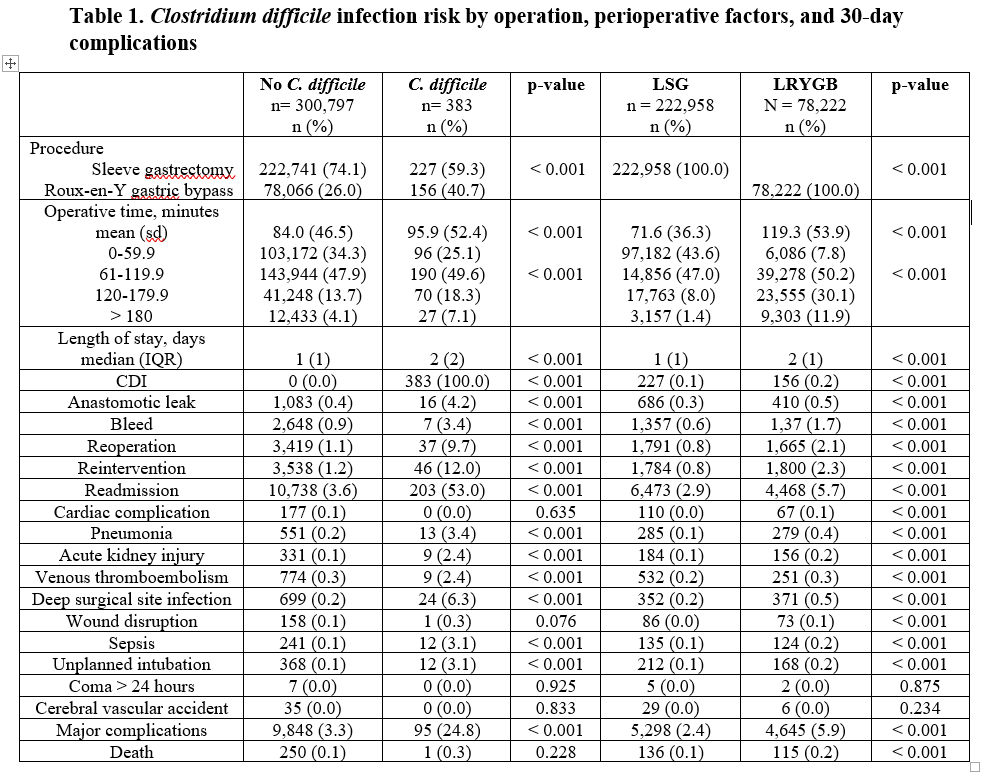
Back to 2019 Posters




