ENTERIC CROHN'S DISEASE - ARE FISTULAS AND STRICTURES ALL THAT DIFFERENT?
Vladimir Bolshinsky*, Awad Jarrar, Alexandra Aiello, Jeremy M. Lipman, Luca Stocchi, Sherief Shawki, Tracy L. Hull, Scott Steele
Colorectal Surgery, Cleveland Clinic, Cleveland Heights, OH
In the era of biologic therapy for IBD, classification of Crohn's disease by phenotype is of increasing significance. As per the Montreal Classification, intestinal manifestations of Crohn's are classified by location and behavior. Stricturing disease is defined as constant luminal narrowing, whilst penetrating disease is defined as occurrence of intraabdominal fistulas, inflammatory masses or abscesses.
The aim of this project is to investigate if stricturing Crohn's disease may be associated with proximal fistulization. Secondary outcomes are to assess if fistulas are associated with visceral location of Crohn's, type of stricture, presence of perianal disease, bowel resection and smoking status.
Following IRB approval, we assessed the prospectively maintained Crohn's Disease hospital database. All operative interventions for Crohn's enteric fistulas were identified (1995 - 2016). Operative notes and histology reports for cases where an intervention was performed for both penetrating and stricturing Crohn's were manually reviewed and statistically analyzed.
Crohn's stricture was defined as site of intestine with evidence of proximal bowel dilatation. Strictures were differentiated as inflammatory, fibrostenotic, or anastomotic/stricturoplasty site. Perianal and pelvic pouch-associated fistulas were excluded.
191 operative cases were identified where surgery was performed for concurrent Crohn's enteric fistula and stricture. There was no evidence of malignancy in any of the fistulas. Fistulas associated with fibrostenotic strictures appeared to be proximal to the stricture site (68%), while fistulas associated with inflammatory strictures were at the stricture (63%) p<0.001. The location of the fistula did not demonstrate a significant association with stricturing p=0.055. Smoking or perianal Crohn's did not have a statistically significant association with enteric fistulas.
Fistulas at index laparotomy were more likely to be associated with concurrent strictures as compared to synchronous, unrelated pathology (p<0.001), however, a difference between inflammatory and fibrostenotic stricutres, or the origin of the fistula in relation to the stricture (at stricture, proximal to stricture, not associated) was not evident. 62 cases had a previous anastomosis, or stricturoplasty. In 37% of these cases a clear relationship between the site of visceral Crohn's and fistula track was not identified.
The results demonstrate that inflammatory strictures appear to predispose to fistulas at the stricture site, where proximal bowel dilatation may be associated with acute inflammation. Fibrostenotic strictures appear to be associated with proximal fistula formation. This may be due to chronic bowel dilatation. Understanding this pattern of disease may prompt earlier surgical review and intervention in order to avoid fistulization and preserve enteric length.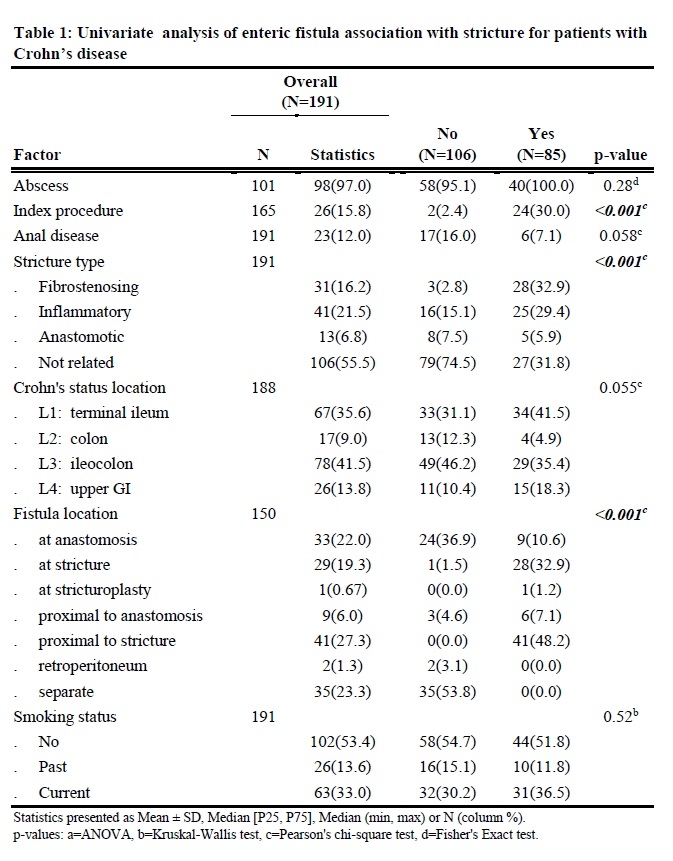
Back to 2019 Posters




