GASTROINTESTINAL STROMAL TUMOR OF THE RECTUM WITH METASTASIS TO THE LIVER IN A PATIENT WITH HIGH GRADE ENDOMETRIAL CARCINOMA: REPORT OF AN UNUSUAL CASE
Priya Gupta*1, Megha V. Patel1, Ronald E. Moore2, Christopher Kowalczyk1
1Dr. Kiran C Patel College of Osteopathic Medicine at Nova Southeastern University, Davie, FL; 2General Surgery, Broward Health Medical Center, Fort Lauderdale, FL
Introduction: Gastrointestinal Stromal Tumors (GIST) are the most common type of mesenchymal neoplasms of the gastrointestinal (GI) tract, yet only account for 1% of all primary GI cancers. Most occur in the stomach or small intestine, but rectal GIST account for only 4% of all cases. The aggressiveness and malignant potential of GISTs are highly variable based on size, location and mitotic activity, but advances in molecular profiling have helped develop targeted chemotherapy to improve prognosis in patients with this mesenchymal neoplasm.
Case Description: Here we present a case of an 82-year-old Caucasian female who initially presented to her gynecologist with postmenopausal vaginal bleeding and anal pressure for 6 months. The patient was referred to gynecologic oncology, where further workup revealed a large pelvic mass and several hepatic hypodensities most likely consistent with metastasis. Subsequent biopsy revealed GIST of the rectum metastatic to the liver. Immunohistochemistry demonstrated a spindle cell neoplasm positive for CD34, CD117 and caldesmon, but negative for PDGFRa mutations. The patient opted to undergo elective surgery involving total abdominal hysterectomy, bilateral salpingo-oophorectomy and resection of the pelvic mass. Deep pelvic exploration during resection of the rectal GIST indicated the need for a Hartmann procedure and creation of an end colostomy. Re-anastomosis was not possible due to the fact that only 2 cm of the rectal stump remained. Surgical pathology revealed high-grade endometrial carcinoma as well as a high-grade GIST of the 12.3 cm pelvic tumor arising from the rectal wall with benign pelvic and iliac lymph nodes. With an uncomplicated post-operative course, the patient was discharged with instructions to follow-up with surgery, gynecology and oncology. Because this patient's GIST was positive for CD34 and CD117 with an exon 11 KIT mutation that is characteristically more responsive to tyrosine kinase inhibitor therapy, oncology recommended starting adjuvant chemotherapy with imatinib for at least 6 months, as well as seeking out clinical trials at tertiary cancer centers for her unique clinical diagnosis.
Conclusion: This case highlights a unique presentation of rectal GIST metastatic to the liver, in conjunction with high grade endometrial carcinoma. Treatment included surgical resection, adjuvant imatinib, and ongoing clinical trials. A clinical hallmark our patient exemplified is the fact that many pelvic GISTs initially present as gynecologic malignancies, frequently leading to misdiagnoses and differentials that exclude mesenchymal neoplasms of the GI tract. Our case also demonstrates the utility of current treatment guidelines recommending resection of large tumors that are symptomatic. Advances in molecular profiling that allow for tailored chemotherapy are highlighted here, as well.
Transgluteal CT-guided biopsy of 12.3x9.7x6.3cm necrotic pelvic mass. Patient in prone position.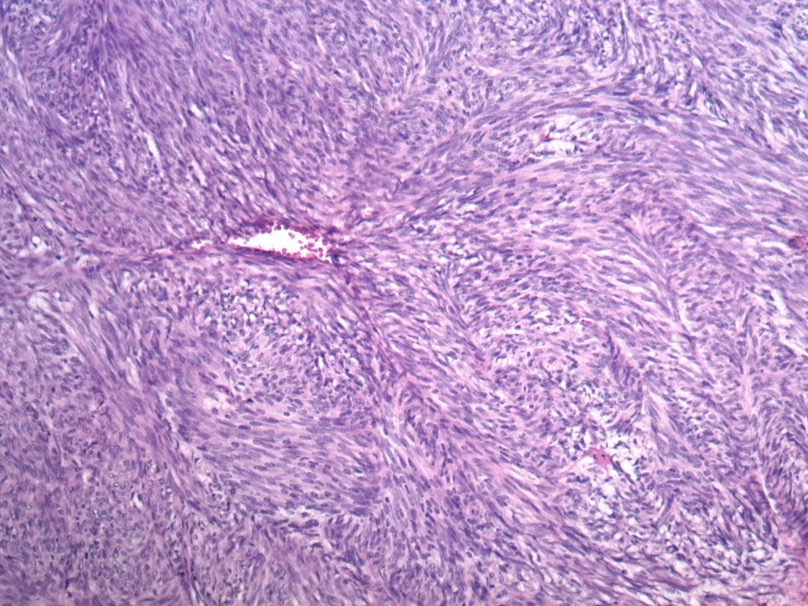
GIST tumor at 100x magnification. This tumor is a cellular spindle cell neoplasm with herringbone and storiform features. Cell are relatively uniform. Mitotic activity is inconspicious.
Back to 2019 Posters




