ILEAL-POUCH ANAL ANASTOMOSIS VOLVULUS: PRESENTATION, MANAGEMENT, OUTCOMES AND FREQUENCY IN A SYSTEMATIC REVIEW AND POOLED ANALYSIS OF THE LITERATURE
Fateh Bazerbachi*1, Muhammad Jawoosh2, Samir Haffar3, Alyssa J. Meyer1, Mohammad Murad5, Amy L. Lightner4, Laura H. Raffals1, David W. Larson4, Navtej S. Buttar1
1Gastroenterology and Hepatology, Mayo Clinic, Rochester, MN; 2Gastroenterology, hepatology & endocrinology, University of Duisburg-Essen, Herne, Germany; 3Digestive Center for Diagnosis and Treatment, Damascus, Syrian Arab Republic; 4Colon & Rectal Surgery, Mayo Clinic, Rochester, MN; 5Division of Health Care Policy & Research, Mayo Clinic, Rochester, MN
BACKGROUND: Proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the procedure of choice for medically refractory ulcerative colitis (UC) and familial adenomatous polyposis (FAP). While rare, a pouch volvulus can occur. Delay in diagnosis is common due to symptoms mimicking small bowel obstruction and pouchitis, and may result in catastrophic complications. We performed a retrospective single center review and systematic review of the literature to determine incidence, natural history, and optimal management of this rare pouch complication.
METHODS: A systematic search of published literature was performed by an experienced librarian on August 10th, 2018, and two reviewers identified relevant papers, extracted data and assessed the methodological quality based on a recently validated tool. Applying the same Boolean search strategy, a retrospective review of the Mayo Clinic electronic medical records of all patients between January 2008 and August 2018 identified one case of pouch volvulus.
RESULTS: A total of 21 patients were identified, with median age 41.2 years (range, 30-71 years); 75% (15/21) were females. The assessment of methodological quality is shown in Figure.1. The indication of IPAA was UC in 85.7% of patients. The primary symptoms included abdominal pain in 76.1% of patients and constipation in 42.8% of patients. The radiologic, endoscopic, and laparoscopic findings demonstrate a long axis twist of the pouch in more than 50% of the cases. A delay in diagnosis occurred in 33.3 % of patients, with 5% completely being missed preoperatively and only identified on laparotomy. The diagnosis was made primarily with computed tomography in 76.1%. Management strategies included laparoscopy in 95.2 % and endoscopic decompression in the remainder. Recurrence of volvulus was reported in 23.8% after endoscopic management. Pouch-pexy was performed in 38%. We summarized in table.1 the main characteristics of total included patients. The frequency of pouch volvulus was reported in one North American retrospective study, wherein 1700 IPAA patients were reported and only 3 experienced volvulus (0.18%).
CONCLUSION: Pouch volvulus is a rare but serious complication of IPAA, and should be included in the differential diagnosis of any patient with symptoms suggestive of bowel obstruction. Heralding signs and symptoms, such as pouch ulceration, ischemia and acute obstipation, should initiate a prompt workup for a twisted pouch. Prompt and early application of barium enema, endoscopy or cross-sectional imaging should be pursued, and salvage surgical pouch detorsion and pexy has good outcomes if performed early.
Table.1: Clinical summary of 21 patients with Ileal-pouch anal anastomosis (IPAA) volvulus
| Age in years (median & range) | 41 (30-71) |
| Females % | 71% |
| Ethnicity | Caucasian 81% - Asian 15% - Indian 5% |
| IPAA indication | UC 86% - FAP 9.5% - rectal cancer 5% |
| Volvulus axis | Longitudinal 67% - Transverse 5% - Not reported 28.5% |
| Clinical manifestations | abdominal pain 76% - nausea 14.2% - vomiting 42.8% pyrexia 14.2% - abdominal distension 43% -constipation 43% - metabolic acidosis 5% |
| Complications (pre- volvulus intervention) | 5 complications (19%): perforation (2) - ischemia (1) - small bowel obstruction (1) - septic shock (1) |
| Associated conditions | pelvic endometriosis 5% |
| Pouch type | J pouch 86% - W pouch 5% - S pouch 5% |
| Diagnostic modality | abdominal x-ray 43% - Gastrografin enema 52% - CT 81% - endoscopy 86% - laparoscopy 95% |
| Surgical interventions | pouch-pexy 33% - pouch excision 33% - devolvulation 19% |
| Surgical complications after laparoscopy | 5 complications (19%): perforation (2) - ischemia (1) - small bowel obstruction (1) - septic shock (1) |
| Follow-up post volvulus intervention (months, median, range) | 22.9 (0.5-60) |
| Mortality | 0 % |
| Interval between IPAA surgery and occurrence of volvulus (months, median, range) | 73 (2-180) |
CT: computed tomography - FAP: familial adenomatous polyposis - IPAA: ileal pouch-anal anastomosis - UC: ulcerative colitis.
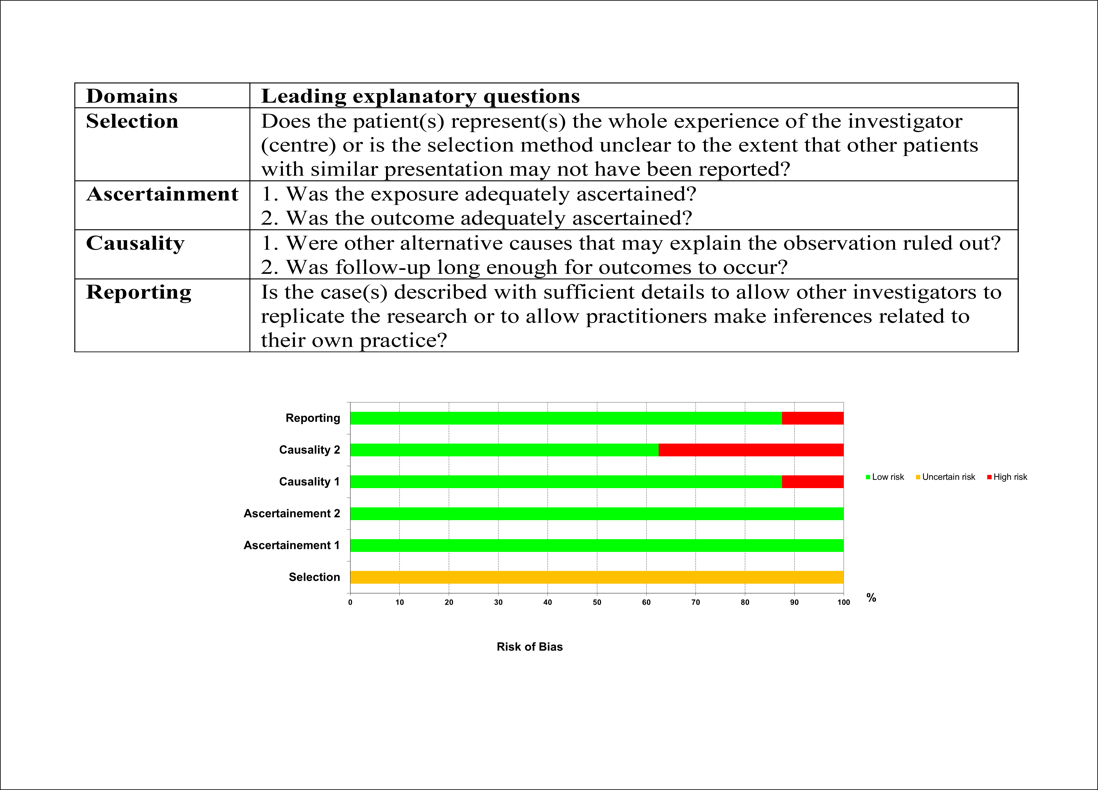
Figure.1 Assessment of methodological quality of included series using the validated tool published by Murad, M. H., Sultan, S., Haffar, S., & Bazerbachi, F. (2018). Methodological quality and synthesis of case series and case reports. BMJ evidence-based medicine, ebmed-2017.
Back to 2019 Posters




