EARLY POSTOPERATIVE ERCP AFTER LAPAROSCOPIC CHOLECYSTECTOMY
Julia Kohn*1,2, Kristine Kuchta1, Alexander Trenk1, Woody Denham1, John G. Linn1, Stephen P. Haggerty1, Ray Joehl1, Michael Ujiki1
1Department of Surgery, NorthShore University HealthSystem, Chicago, IL; 2University of Illinois at Chicago College of Medicine, Chicago, IL
INTRODUCTION
Despite the prevalence of laparoscopic cholecystectomy, there is still debate about how to manage the possibility of choledocholithiasis intraoperatively. Many physicians do not routinely perform intraoperative cholangiography (IOC), but missing a retained common bile duct stone could subject patients to further illness and a second procedure after surgery, commonly ERCP. Evaluating predictors of early postoperative ERCP may identify characteristics of patients who require intraoperative common bile duct evaluation or intervention.
METHODS
After IRB approval, a database of 900 randomly selected cholecystectomies performed between 2009 and 2015 at NorthShore University HealthSystem was created, containing pre-, intra-, and postoperative data. All operative notes and ERCP documentation were individually reviewed. Acute surgery was defined by patients undergoing inpatient surgery, rather than elective procedures. Following preliminary analysis, multivariable logistic regression with a backward selection method was used to identify predictors of IOC and of ERCP within 1 week of surgery (early postoperative ERCP).
RESULTS
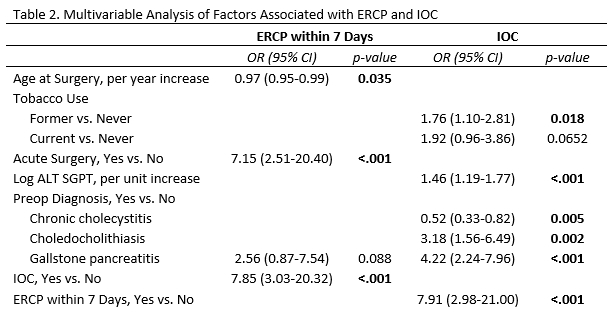
Of 900 patients undergoing cholecystectomy, 112 had IOC, performed at the surgeon's discretion. Twenty-two underwent ERCP within 7 days postoperatively (findings, table 1); two patients had a cystic duct stump leak, and one patient had an incomplete study. Early ERCP was associated with younger patients, acute surgery, and intraoperative cholangiography (table 2). IOC was associated with previous tobacco use, preoperative ALT, a preoperative diagnosis of choledocholithiasis or pancreatitis, and early postoperative ERCP (table 2). Other common predictors of choledocholithiasis, including elevated serum bilirubin and common bile duct dilation on preoperative CT or ultrasound, were not independently associated with IOC or postoperative ERCP.
DISCUSSION
Early postoperative ERCP was not associated with clearly delineated preoperative factors. However, IOC is associated with preoperative characteristics suspicious for choledocholithiasis; given that IOC is not routinely performed by the surgeons whose cases make up 97% of this database, these findings may represent efforts to evaluate and address choledocholithiasis during cholecystectomy. The association between early postoperative ERCP and IOC suggests that surgeons may prefer ERCP for management, rather than attempting to address the common bile duct intraoperatively. Previous research in this patient cohort demonstrated an association between acute inflammation and common bile duct injury; surgeons could therefore be choosing ERCP to reduce this risk in patients undergoing acute surgery. Assessing decision-making surrounding IOC and ERCP, as well as surgeon comfort with intraoperative common bile duct exploration, may further clarify factors that lead to postoperative ERCP.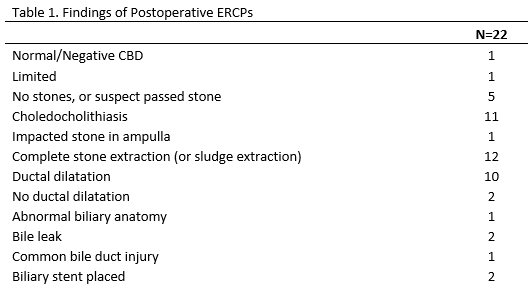
Back to 2019 Posters




