FUNCTIONAL GASTROINTESTINAL AND NEUROLOGIC DISORDERS MAY ALTER GASTROESOPHAGEAL REFLUX DISEASE PRESENTATION AND POST-OPERATIVE SYMPTOMOLOGY AND QUALITY OF LIFE FOLLOWING NISSEN FUNDOPLICATION
Anahita D. Jalilvand*, Patricia Belle, Monet McNally, Kyle A. Perry
General Surgery, Ohio State Medical Center, Hilliard, OH
INTRODUCTION: The impact of functional gastrointestinal and neurologic disorders, including fibromyalgia (FM) and irritable bowel syndrome (IBS), on surgical management of gastroesophageal reflux disease (GERD) is unclear. The goal of this study was to compare preoperative symptomology and objective work-up and patient reported outcomes of GERD symptom control and disease-specific quality of life (QoL) in patients with and without baseline IBS/FM diagnoses following laparoscopic Nissen fundoplication (LNF). We hypothesized that patients with IBS/FM would have equivalent improvement in GERD symptoms and QoL to those without these conditions.
METHODS: A retrospective cohort study of all patients undergoing LNF from 2011-2017 at a single institution (n=314) was performed. Patients were grouped by presence of a baseline diagnosis of either IBS or FM (IBS/FM n=27, Control N=276). Data collected included demographic data, presenting symptoms, objective testing and follow-up symptoms, which are maintained in an institutionally approved database. Primary outcomes included baseline and follow-up GERD-health related QoL (GERD-HRQL) and symptom scale (GERSS) scores at a median follow up of 6-18 months. Secondary outcomes included post-operative antacid usage and endoscopic dilation. Statistical analysis was performed using Stata 12 (College Station, TX) and a p value of 0.05 was considered statistically significant.
RESULTS: There was no difference in mean age or baseline BMI between groups, but IBS/FM patients were more likely female (96% vs 31%, p=0.001). Patients with IBS/FM more frequently presented with globus sensation (48% vs 24%, p=0.01) and cough (48% vs 28%, p=0.05). The IBS/FM group had increased baseline DeMeester score of 47 (33-62) compared to 37 (26-55) in the control group (p=0.25). Baseline GERD-HRQL (36 (25-41) vs 30 (19-37), p=0.04) and GERSS (44(36-63) vs 38 (24-48), p=0.007) scores were significantly higher in the IBS/FM group. Both groups demonstrated significant post-operative reductions in GERD-HRQL and GERSS scores post-operatively and these did not differ between groups (Table 1). Post-operative antacid use and need for endoscopic dilation were comparable between groups. Patient reported dysphagia (1 vs 0, p=0.50) and bloating (3 vs 2, p=0.17) scores did not differ between groups.
CONCLUSION: In this study, patients with IBS/FM presented with higher baseline GERD-HRQL and GERSS scores and more frequently reported atypical GERD symptoms compared to patients without these diagnoses. Despite these differences, these patients demonstrated comparable post-operative relief without significantly increased postoperative bloating. However, given the trend toward mildly increased post-operative bloating and dysphagia, larger studies are needed to elucidate subtle differences between the outcomes in these patient populations.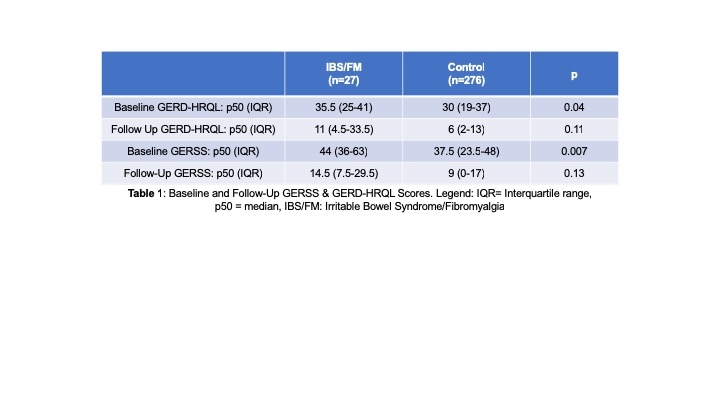
Back to 2019 Posters




