OVERWEIGHT AND OBESITY IN THE LONG TERM AFTER HELLER MYOTOMY
Sofia Narvaez-Chavez*3, Janette Furuzawa-Carballeda2, Enrique Coss-Adame4, Miguel A. Valdovinos4, Fidel López-Verdugo2, Hector Olvera-Prado3, Jose Peralta-Figueroa3, Emilio Sanchez- Garcia Ramos1, Oscar Santes1, Angélica Rodríguez-Garcés3, Fernanda Romero-Hernández3, Gonzalo Torres-Villalobos3
1Surgery, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico, Distrito Federal, Mexico; 2Inmunologia y Reumatologia, Instituto Naciona de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Mexico; 3Cirugia Experimental, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico city, Mexico; 4Gastroenterology, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Mexico
Background and Aims
Resolution of dysphagia in achalasia patients after laparoscopic Heller myotomy (LHM) may lead to weight gain. There are no studies about the changes on weight or body mass index (BMI) in achalasia patients before and after LHM. To better understand those weight variations, we evaluated pre-surgical and long-term BMI after LHM and identified if BMI categories influence symptom scores questionnaires, high resolution manometry (HRM) or 24-h pH monitoring.
Methods
This was an observational study including achalasia patients with diagnosis made by HRM, upper endoscopy and barium esophagogram. Data was obtained from a prospective database and medical records. Usual BMI was defined as the BMI prior to achalasia symptoms. Before surgery, the GERD-HRQL, EAT-10 and ECKARDT questionnaires were obtained and HRM was performed.
All patients underwent LHM plus partial fundoplication. During follow-up, the same questionnaires were applied, calculating the BMI and HRM at 1, 6, 24 and 48 months. At 6, 12, 24 and 48 months a 24 hours pH monitoring was performed.
Results
We included 113 patients (table 1). Mean usual BMI was 28.85 ą 6.61 and mean BMI in the immediate preoperative period decreased to 23.02 ą 4.6 (p <0.05). Before symptoms 33% patients had overweight and 33% were obese. The number of overweight and obese patients in the immediate preoperative period decreased to 20.7% and 6%, respectively. Overall, there was significant weight loss between usual BMI and BMI at 1, 6 and 24 months (p <0.05). During post-surgical follow-up, the percentage of overweight and obese patients increased to 28.5% and 5% at the first month, 40% and 8% at 6 months, 40% and 30% at 24 months and 47% and 30% at 48 months, respectively (figure 1).
Of the 30 patients with usual obesity, 30% recovered their usual BMI at 6 months, while 66% recovered at 24 months. The 2 patients with persisting BMI ≥35 in the immediate preoperative period remained in this category in the postoperative follow up.
Overall BMI at 48 months was similar compared to the usual BMI (p = 0.088). Statistically significant correlation was found between the weight gained at 24 months, and weight gained at 48 months (r = 0.97, p <0.05). There were no differences for symptom questionnaires, HRM and 24-h pH monitoring for any of the follow-up visits between BMI categories.
Conclusions
The percentage of patients with obesity at 48 months after surgery was the same as the usual BMI. The percentage of patients with overweight increased at 48 months compared to the usual BMI. These indicate that the risk of excessive weight gain after surgery is present. It's necessary to maintain strict surveillance over those patients due to their risk of developing obesity and overweight. BMI does not seem to influence the symptom scores questionnaires, the manometric parameters or the 24-h pH monitoring in the long term.
Table 1. Baseline demographic, clinical and HRM characteristics.
| Demographic | Gender Female, n(%) | 69 (61.1) |
| Age, meanąSD (years) | 40.95ą14.82 | |
| Type of achalasia | I, n(%) | 32 (29.9) |
| II, n(%) | 73 (68.2) | |
| III, n(%) | 2 (1.9) | |
| Clinical variables | Disease duration, median (IQR) (months) | 18 (8-36) |
| Height, meanąSD (m) | 1.61ą0.92 | |
| Usual weight, meanąSD (kg) | 75.58ą18.42 | |
| Weight in the immediate preoperative period, meanąSD (kg) | 60.91ą14 | |
| Weight loss, meanąSD (kg) | 14.59ą10.8 | |
| BMI in the immediate preoperative period, n(%) | ||
| Underweight (<18.5) | 16 (16.3) | |
| Normal (18.5-24.9) | 55 (56.1) | |
| Overweight (25-29.9) | 21 (21.4) | |
| Obesity (>30) | 4 (6.1) | |
| Pre-surgical symptoms | GERD-HRQL, meanąSD | 24.12ą12.62 |
| EAT-10, meanąSD | 29.31ą9.43 | |
| Eckardt, meanąSD | 8.97ą2.84 | |
| High resolution manometry | Integrated relaxation pressure, meanąSD (mm Hg) | 29.1ą14.36 |
| Basal lower esophageal sphincter pressure, meanąSD (mm Hg) | 40.92ą25.63 |
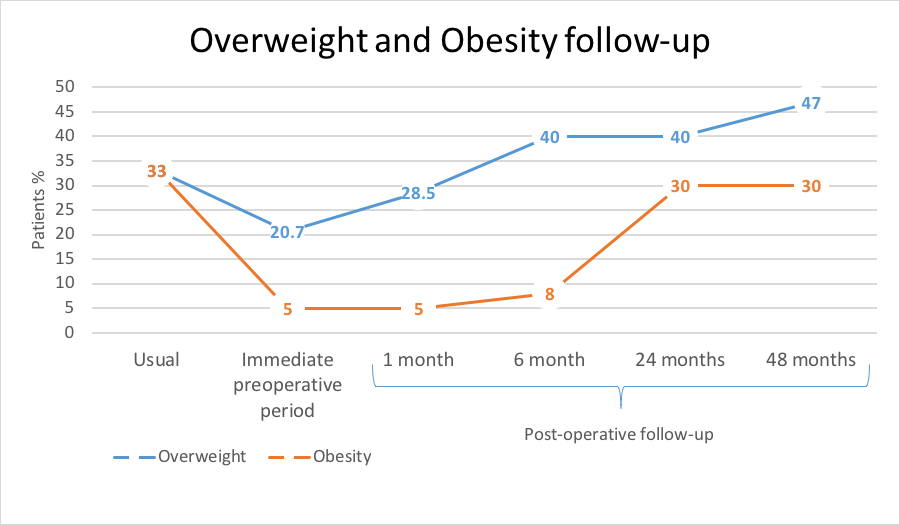
Figure 1. BMI long-term follow up.
Back to 2019 Posters




