TGF-β TREATMENT IS ASSOCIATED WITH A DECREASE IN METASTATIC POTENTIAL BUT INCEASED C-MYC EXPRESSION IN PANCREATIC ADENOCARCINOMA CELL LINES
Marcus A. Alvarez*1, Yongchao Li2, Syed M. Hussain1, Evan S. Glazer1
1General Surgery, University of Tennessee - Health Science Center, Memphis, TN; 2Pathology, University of Tennessee - Health Science Center, Memphis, TN
Introduction: Pancreatic ductal adenocarcinoma (PDAC) is expected to become the second leading cause of cancer death over the next decade. TGF-β is an inflammatory mediator that is known to play a role as both a tumor promoter and suppressor in the pathogenesis of PDAC through various pathways. c-MYC is an oncogene whose overexpression has been found in both primary and metastatic pancreatic cancer. We hypothesize that TGF-β treatment of PDAC cell lines would result in alterations in the characteristics of primary and metastatic tumors in an orthotopic murine model and changes in c-MYC expression.
Methods: In order to evaluate the effects of TGF-β on PDAC pathogenesis, Panc-1 cells (derived from primary PDAC), gemcitabine resistant Panc-1 cells (selected for by increasing gemcitabine exposure over 6 months), and Capan-1 cells (derived from metastatic PDAC) were treated with recombinant TGF-β (10 ng/mL) vs. a PBS control. The treated cells were then orthotopically implanted into the pancreas of NOD scid gamma mice (NSG) with 5 mice per group. After 6 weeks the mice were sacrificed and evaluated for primary tumor weight and number of surface liver metastases and compared using Student's t-Test. In these same cell lines c-MYC expression was evaluate by Western Blot analysis.
Results: After sacrifice the pancreatic tumors weights were not different in the TGF-β treated cells vs. the PBS treated cells 1.04 vs. 1.18 g (p=0.51). The number of liver surface metastases were significantly decreased across all cell lines exposed to TGF-β vs. PBS controls- 2.0 vs. 6.8 metastases respectively (overall p=0.008). Among the subgroups, Panc-1 and gemcitabine resistant Panc-1 cells showed a significant decrease in liver surface metastases in those treated with TGF-β vs. PBS (2.8 vs 7.4, p=0.021 and 1.8 vs. 6.8, p=0.024); there was no significant changes in liver metastasis in the Capan-1 tumors (1.6 vs. 2.3, respectively, p=0.51). In protein analysis, we found that TGF-β significantly increased the protein expression of c-MYC in Capan-1 cells, without a definitive change in Panc-1 or gemcitabine resistant Panc-1 cells.
Conclusion: We found that treatment of cell lines with TGF-β resulted in fewer liver surface metastases in vivo when compared to control. Paradoxically, in our protein analysis, TGF-β increased expression of c-MYC in both Panc-1 and Capan-1 cell lines, though the difference was more profound in Capan-1 than Panc-1 cells. We will study long-term TGF-β exposure of patient derived PDAC to investigate if that will yield rising c-MYC expression and eventually a tumor promotive phenotype.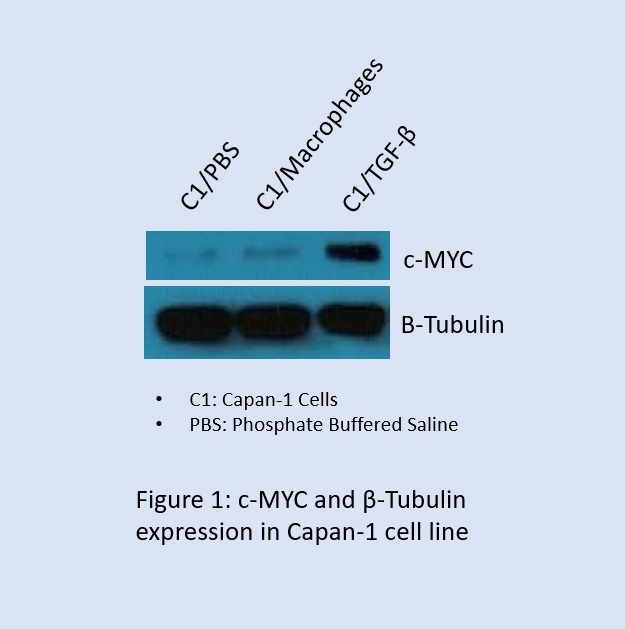
Back to 2019 Posters




