IS PROVIDER DENSITY ASSOCIATED WITH UTILIZATION OF SURGICAL CANCER CARE?
David Xiao*1,2, Alexander Zeymo1,3, Kitty Chan1,3, Kelsie M. Gould1,2, Thomas J. Watson4,5, Waddah Al-Refaie1,4,3
1Medstar-Georgetown Surgical Outcomes Research Center, Washignton, ; 2Georgetown University School of Medicine, Washington, ; 3MedStar Health Research Institute, Washington, ; 4Medstar-Georgetown University Department of Surgery, Washington, ; 5Georgetown University Medical Center, Washington,
Background:
Deeper understanding of the complex interplay between providers and access to quality surgical care has been recognized as a key mechanism in reduction of surgical disparities. While increased provider density has predicted improved cancer outcomes in select cancers, its impact on access to surgical cancer care is not well understood. This study aimed to measure the effects of primary care and specialist provider density on utilization of surgical cancer care overall and at high volume hospitals (HVH).
Methods:
Using the Healthcare Cost and Utilization Project-State Inpatient Database, we identified 122,646 patients aged 18 and older in 5 states (KY, MD, NC, NJ, and FL) who underwent inpatient resections for one of three common surgical cancers (rectal, pancreatic, or lung) from 2012-15 Q3. We examined the distribution of primary care physician (PCP) and specialist density within counties (based on where patients lived) and tested for associations with utilization rates of cancer surgeries. We used multivariate Poisson regression models to assess the impact of provider density on the adjusted incidence rate ratio (IRR) of overall surgical utilization and adjusted odds of utilization of HVH (high volume=top quintile) for surgery.
Results:
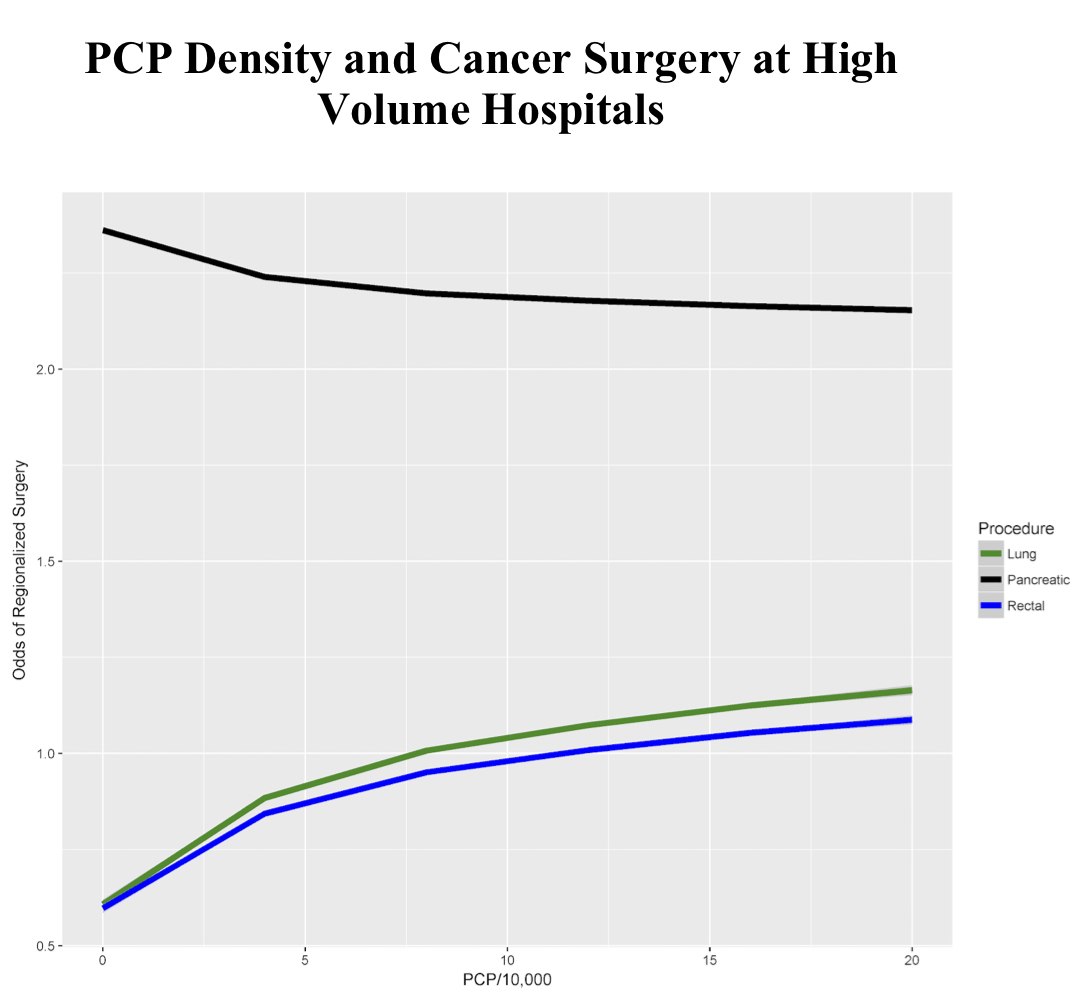
PCP density was associated with greater overall surgery utilization in pooled analysis with adjusted IRR of 1.056 and 1.026 for the 3rd and 4th quartiles, respectively. By cancer site, PCP density showed a positive association with utilization only for rectal cancer surgery with adjusted IRR of 1.069 and 1.028 for the 3rd and 4th quartiles, respectively. PCP density increased odds of utilization of cancer surgery at HVHs in pooled analysis with an adjusted OR of 1.15. In stratified analysis, the relationship was prominent for lung and rectal cancer surgery (adjusted OR of 1.176 and 1.161, respectively) but not for pancreatic cancer surgery (Figure). Specialist density did not impact the use of HVHs for major cancer surgery overall. When stratified, only rectal cancer surgery showed specialist density (colorectal and general surgeons) associated with greater HVH utilization with an adjusted OR of 1.048 (Table).
Conclusion:
These multi-state analyses showed a mixed relationship between provider density and access to surgical cancer care. Density appears to have a select impact, however, on access to HVHs for surgical cancers. Future research efforts should investigate other mechanisms beyond provider supply that can improve access to quality surgical care, such as referral networks and health systems.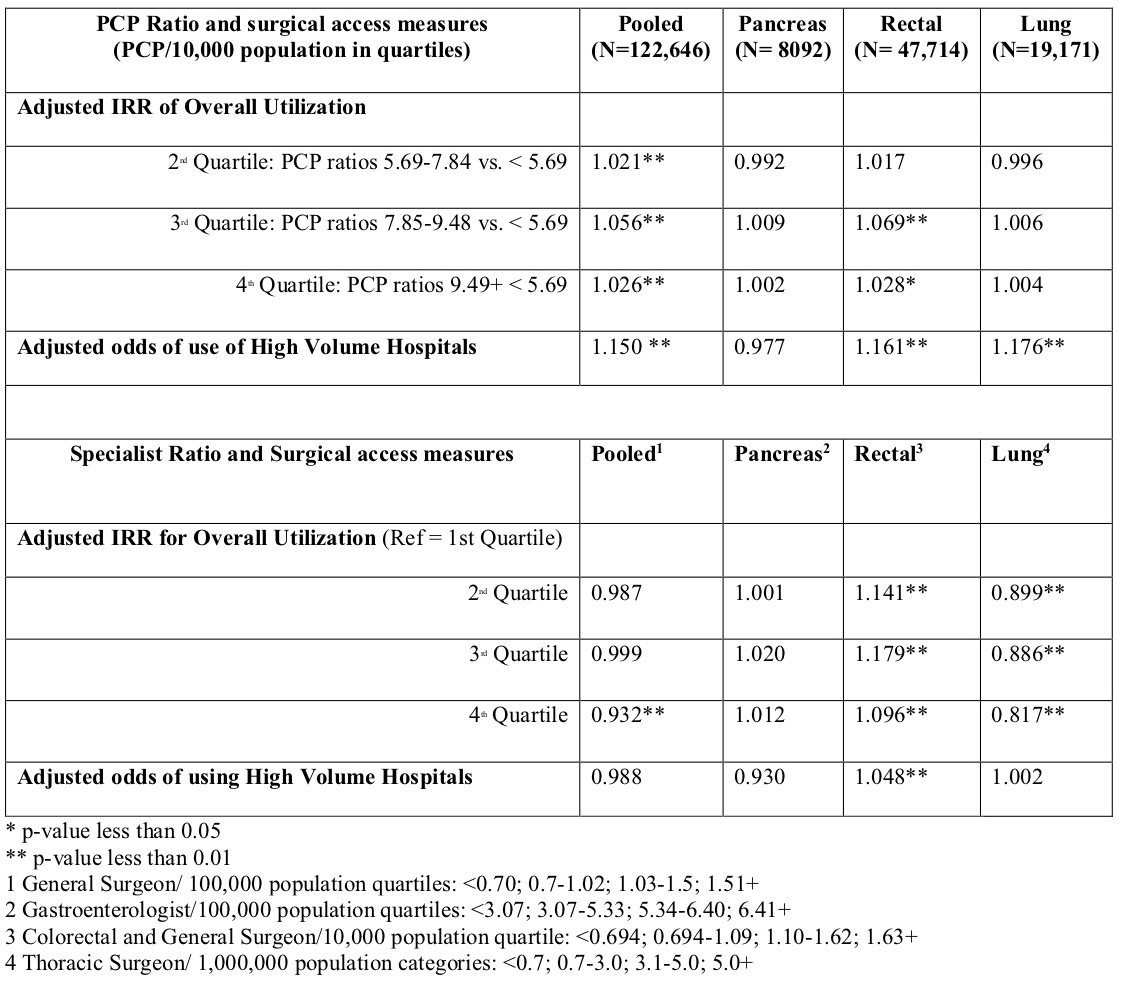
Back to 2019 Posters




