THE EFFECTS OF PROBIOTICS ON SYMPTOM AND SURGICAL OUTCOME AFTER ANTERIOR RESECTION OF COLON CANCER; MULTICENTER, DOUBLE-BLIND, RANDOMIZED, PLACEBO-CONTROLLED TRIAL (POSTCARE STUDY)
In Kyu Lee*1, Bong-Hyeon Kye1, Ju-Hoon LEE2, In Ja Park3, Heung-Kwon Oh6, YONG BEOM Cho4, You-Tae Kim2, Joo Yun Kim5, Jung-Lyoul Lee5, Jae-Hun Sim5
1Sugery, Seoul St. Mary's Hospital, Seoul, Korea (the Republic of); 2Department of Food Science and Biotechnology, Kyung Hee University, Youngin, 17104, Korea (the Republic of); 3Department of Colon and Rectal Surgery, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea (the Republic of); 4Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea (the Republic of); 5R&BD Center, Korea Yakult Co. Ltd, Youngin, Korea (the Republic of); 6Department of Surgery, Seoul National University Bundang Hospital, Bundang, Korea (the Republic of)
BACKGROUND & AIMS
The purpose of this study is to investigate the correlation between microbiota and inflammation related markers due to cancer, mechanical bowel preparation (MBP) and antibiotics, and surgery. We also investigated the effects of probiotics treatment on microbiota and inflammatory changes and surgical outcomes.
METHODS
Sixty-eight patients undergoing anterior resection due to sigmoid colon cancer were enrolled. We obtain final data for 29 patients in probiotics groups (P group) and 30 patients in control group (C group), The patients received probiotics and prebiotics (P group) or prebiotics (C group) twice a day for 4 weeks from 1 week before surgery. We examined anterior resection syndrome (ARS), microbiota in stool, inflammation related markers, zonulin, EORTC QLQ-c30, nutritional screening index at pre-operation, after MBP and surgery (Fig. 1).
RESULTS
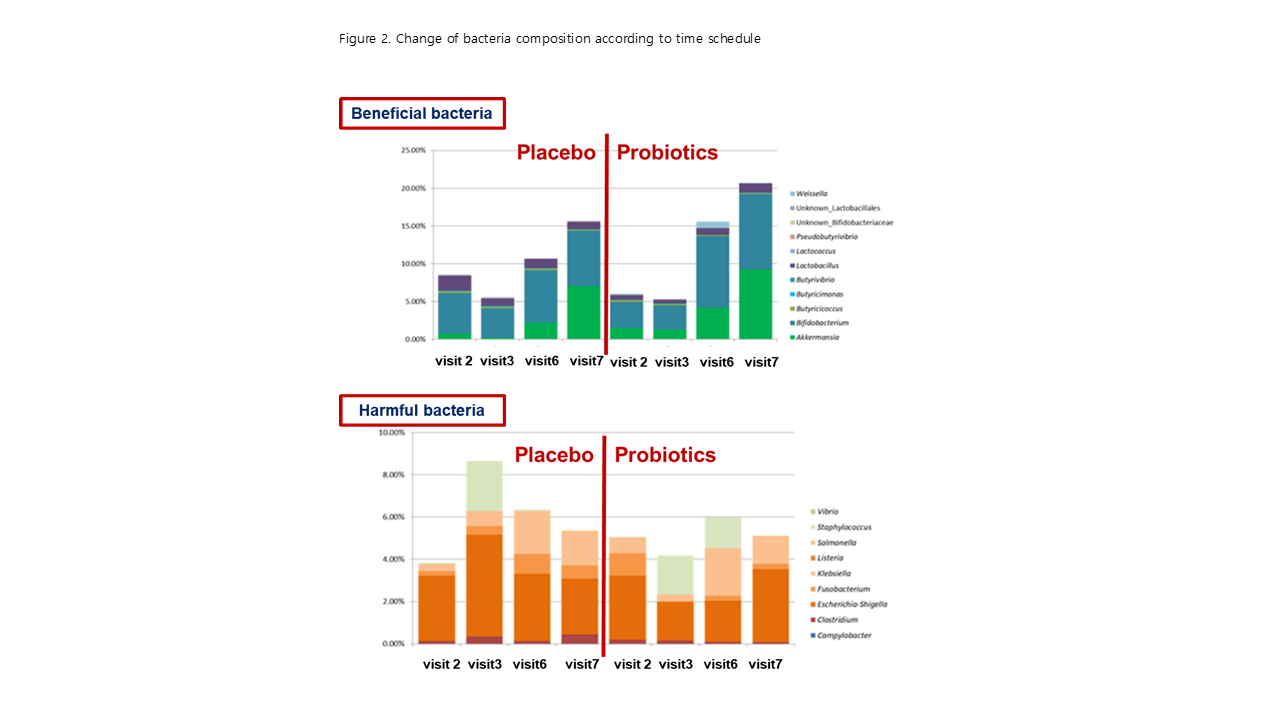
The adverse events after perioperative probiotics and prebiotics ingestion were no significant differences between P group (11 cases) and C group (22 cases). The change in LARS score in group P showed a tendency to improve. (3.3±13.7 vs 10.52±15.7, p=.063), especially flatus(p=.030). Serum zonulin concentration (p = 0.012), neutrophil count (p=.042) and IL-10 (p <0.001) were significantly decreased in the P group. Surgical complications were 1 case in P group and 6 cases in C group in ITT set (P=.112). Two cases of only C group dropped out due to anastomotic leakage and pseudomembranous colitis, respectively. Due to probiotic ingestion, compositions of gut microbiota between P and C groups were changed in different manner (Fig. 2). After antibiotic treatment for surgery, beneficial gut bacteria including Bifidobacterium and Akkermansia became dominant in P group. After surgery, growth of beneficial bacteria was promoted in the disrupted gut microbiota by antibiotics treatment, probably due to ingestion of probiotics and prebiotics (P group) or prebiotics (C group). In addition, growth of harmful bacteria was inhibited probably due to ingestion of probiotics (in visit 2 and 3) and promoted dominance of beneficial bacteria (in visit 6 and 7) in P group. However, the percentage of harmful bacteria increased in C group, because of no ingestion of probiotics in visit 2 and 3.
CONCLUSIONS
First, microbiota was changed in colorectal cancer patients and microbiota changed normally over time by surgery. Second, the preoperative management (MBP and antibiotics) and surgery resulted in changes in microbiota and inflammation related markers. Third, the changes of microbiome and inflammatory response, and surgical complication were decreased by probiotics and the functional improvement was also confirmed.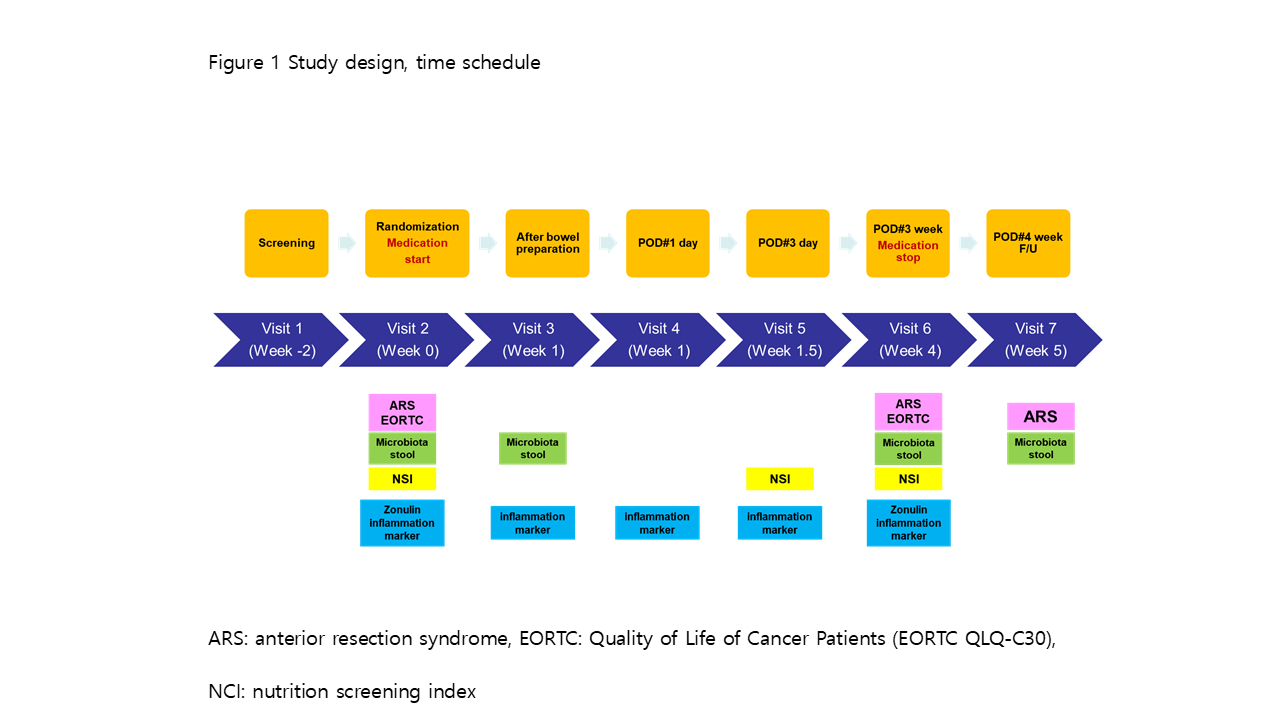
Back to 2019 Abstracts




