VADIS - PROSPECTIVE STUDY FOR VALIDATION OF THE CLASSIFICATION OF DIVERTICULAR DISEASE
Johannes Lauscher*1, Johan Lock2, Andrea Stroux3, Christoph-Thomas Germer2, Martin E. Kreis1
1General, Visceral and Vascular Surgery, Charitè University Medicine Berlin, Berlin, Germany; 2University Hospital Würzburg, Würzburg, Germany; 3Institute for Biometry, Charité University Medicine, Berlin, Germany
Introduction: The Hinchey classification for diverticulitis was developed to guide treatment decisions for acute perforated diverticulitis. It has limitations for chronic recurrent and less severe acute types of diverticular disease. To include less severe types of disease as well as chronic recurrent courses, the classification of diverticular disease (CDD) was introduced (Image 1). To explore if CDD is enables us to differentiate different types of diverticular disease with regard to long-term course and prognosis, the prospective VADIS study was set up.
Materials and methods: The VADIS study was a prospective non-randomized observational bicentric study. Patients were eligible aged 18 years or older with a diverticulosis or diverticular disease proven by CT scan of abdomen and pelvis, abdominal ultrasound or colonoscopy. Follow-up was two years.
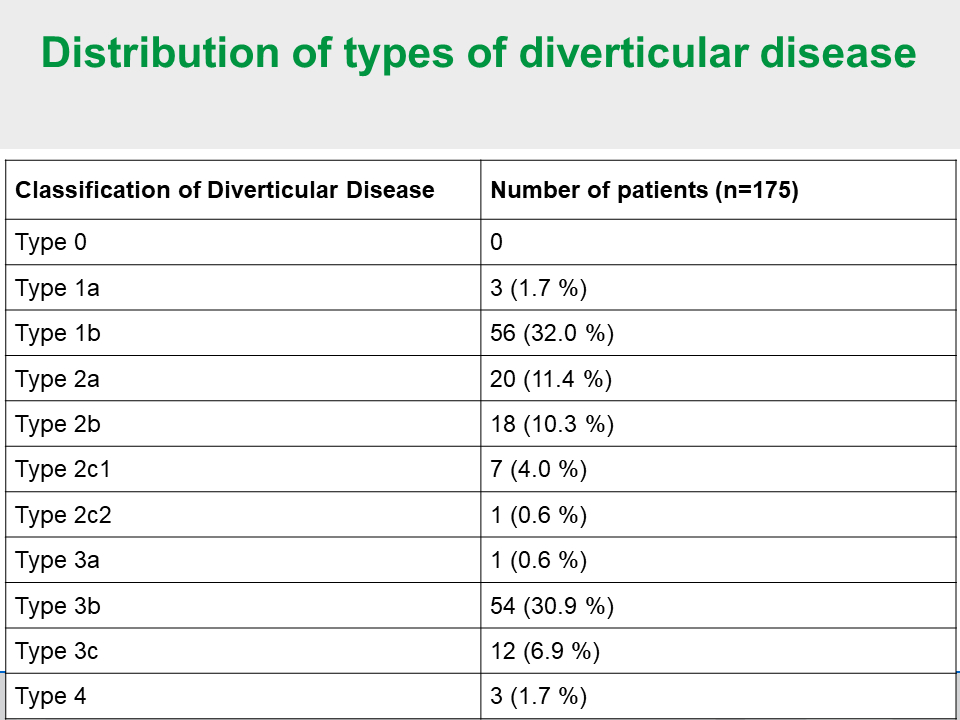
Results: 176 patients were included in the study. Mean age of the study cohort was 61 years, 85 patients were female (48.3 %) and 91 patients male (51.7 %), mean body-mas index was 28.2 kg/m2, 39 patients were smokers (22.2 %), 32 had coronary artery disease (18.2 %), 17 suffered from diabetes (9.7 %). 20 patients were on immunosuppressive medication (11.4 %) and the mean number of episodes of diverticulitis were 3.1. Image 2 illustrates the distribution of patients on the types of diverticular disease according to CDD. Comparison of acute diverticulitis with phlegmonous peridiverticulitis (type 1b) vs. acute complicated diverticulitis with abscess (type 2a and type 2b) showed that surgery on the first hospital stay was performed in four of 56 patients (7.1 %) in type 1b and in 19/38 in type 2a/b (50 %); p<0.001. Hospital stay was 5.6 ± 4.6 days in type 1b and 11.3 ± 7.7 days in type 2a/b; p<0.001. Recurrent diverticulitis within two years follow-up occurred in 11/44 patients (25 %) in type 1b and in 6/27 patients (22.2 %) in type 2a/b; p=0.495. Gastrointestinal quality of life index (GIQLI) after two years follow-up revealed 120.8 ± 16.1 points for type 1b vs. 117.4 ± 15,3 points for type 2a/b. (p=0.319). Comparison of relapsing diverticulitis without complications (type 3b) vs. relapsing diverticulitis with complications (type 3c) showed that surgery on the first hospital stay was performed in 38/54 patients (70.4 %) in type 3b and in 12/12 in type 3c (100 %); p<0.030. Hospital stay was 10.6 ± 6.8 days in type 3b and 19.3 ± 10.1 days in type 3c; p<0.008. GIQLI after two years follow-up revealed 109.5 ± 21.4 points for type 3b vs. 127.5 ± 9.0 points for type 3c; (p=0.073).
Conclusion: The VADIS study provides evidence that the classification of diverticular disease (CDD) may differentiate between uncomplicated and complicated types of acute and chronic recurrent diverticular disease.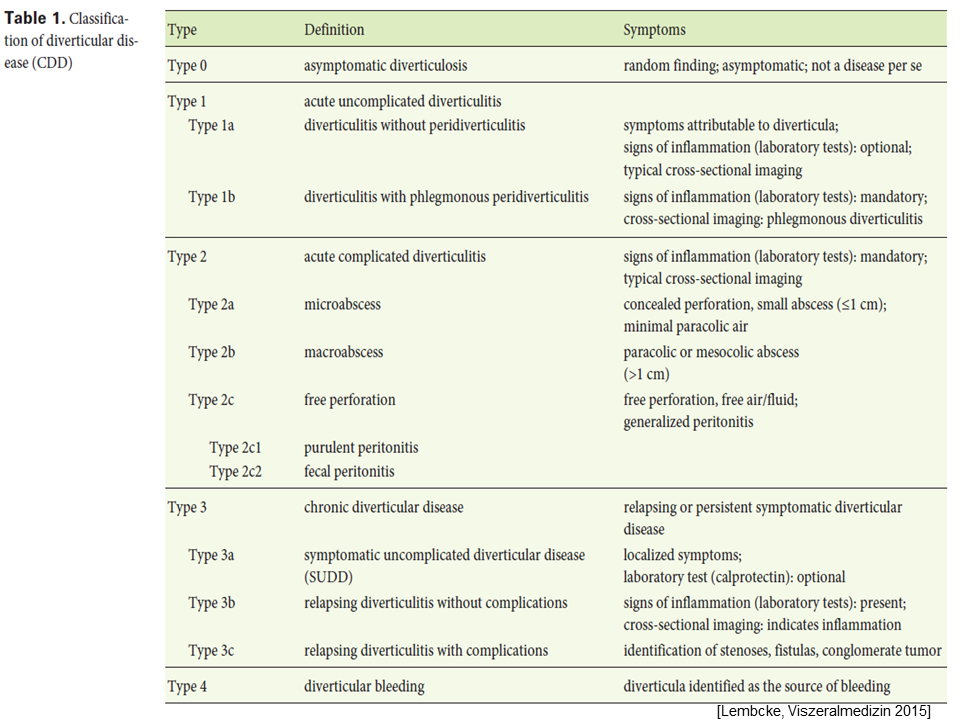
Back to 2019 Abstracts




