ROBOTIC COLECTOMY OUTCOMES HAVE IMPROVED OVER TIME: AN AMERICAN COLLEGE OF SURGEONS NSQIP DATABASE ANALYSIS
John D. Vossler*, Michael K. Rao, Chad Cryer, Dean Mikami, Kenric Murayama
Department of Surgery, University of Hawaii, Honolulu, HI
Objective:
Utilization of robotic-assisted surgery is rapidly increasing for colectomy. New surgical approaches are associated with learning curves. It is unknown if the rate of adverse outcomes has changed with time during the rapid expansion of robotic colectomy. We hypothesize that robotic colectomy outcomes have improved over time.
Methods:
A retrospective analysis of 11,060 robotic colectomy procedures was conducted using the ACS-NSQIP 2013-2017 colectomy targeted procedure database. Univariate comparison of preoperative demographics, comorbidities, and post-operative outcomes were compared between years by Chi-squared test. Risk adjusted odds ratios of adverse outcomes for each year relative to 2013 were calculated by multivariate logistic regression using models created by stepwise minimization of AIC. Statistical significance was assigned to p-values < 0.05. Statistical analysis was performed using R version 3.5.1.
Results:
Univariate analysis of pre-operative variables and outcomes is presented in Table 1. The pre-operative variables with statistically significant differences between years were race, obesity, and ASA classification. Race distribution varied from year to year in a statistically, but not clinically, significant fashion. The percentage of obese patients increased abruptly from 2013 to 2014 and then remained relatively constant through 2017. ASA classification distribution gradually shifted toward higher ASA class from 2013 to 2017. Overall morbidity, wound complication, and unplanned conversion to open rates gradually declined from 2013 to 2017. No other pre-operative variables or outcomes had a statistically significant difference between years.
Multivariate analysis of adverse outcomes is presented in Table 2. Patients in 2016 and 2017 were less likely to experience an overall morbidity or wound complication than patients in 2013. Patients in 2014, 2015, 2016, and 2017 were less likely to experience an unplanned conversion to open than patients in 2013. No adverse outcomes increased in likelihood from 2013 to any subsequent year.
Conclusions:
The results presented support our hypothesis that robotic colectomy outcomes have improved over time. Specifically, overall morbidity, wound complication, and unplanned conversion to open rates have improved with time on a national level. It is reasonable to infer that a similar learning curve has also occurred at the level of individual surgeons and institutions. We conclude that one must anticipate that the early experience of a surgeon or institution with robotic colectomy will go through a learning curve, and that a surgeon with below average outcomes who fails to see improvement in overall morbidity, wound complications, and unplanned conversion to open over their first 5 years should reconsider their use of robotic-assisted surgery for colectomy.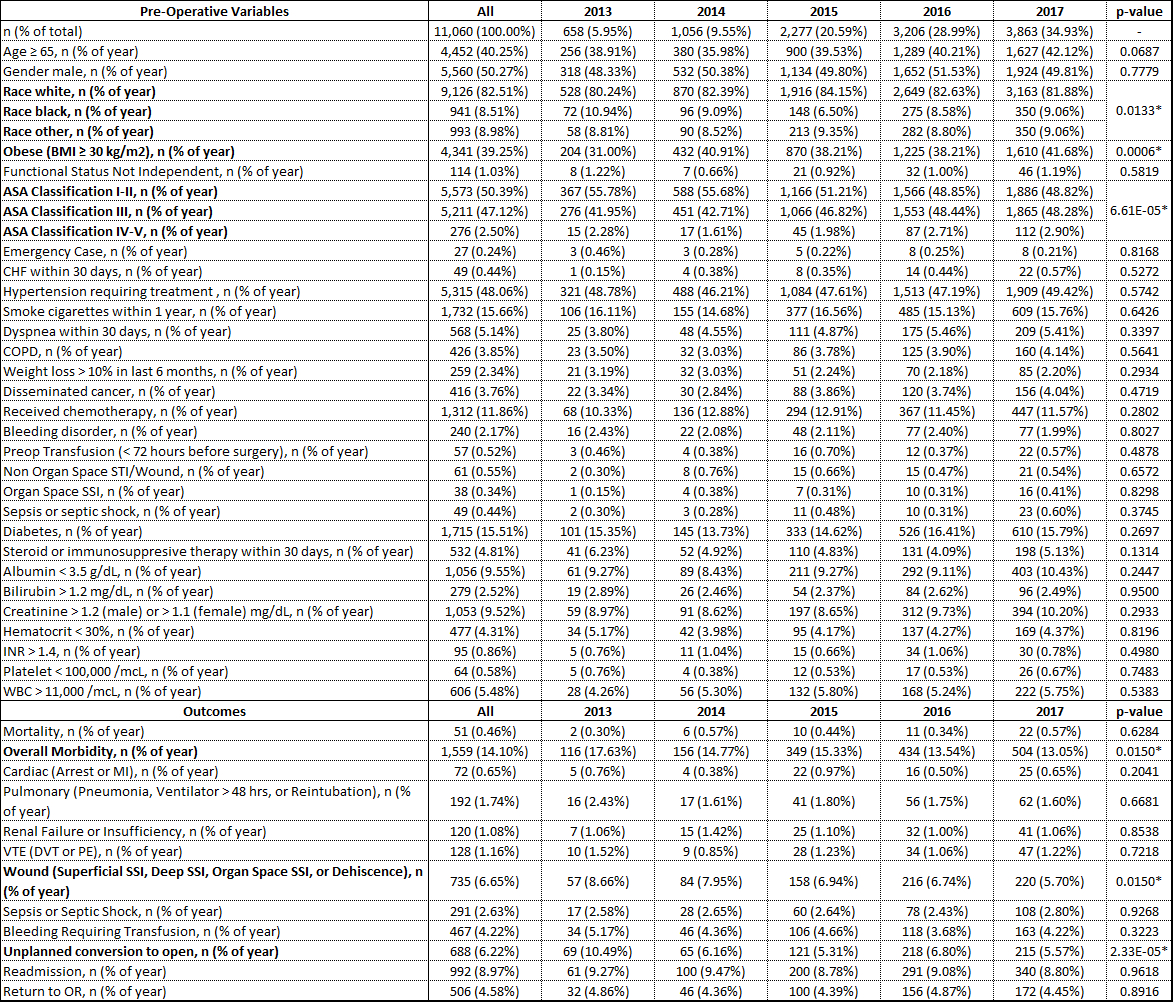
Table 1. Univariate comparison of pre-operative variables and outcomes by year. *p < 0.05.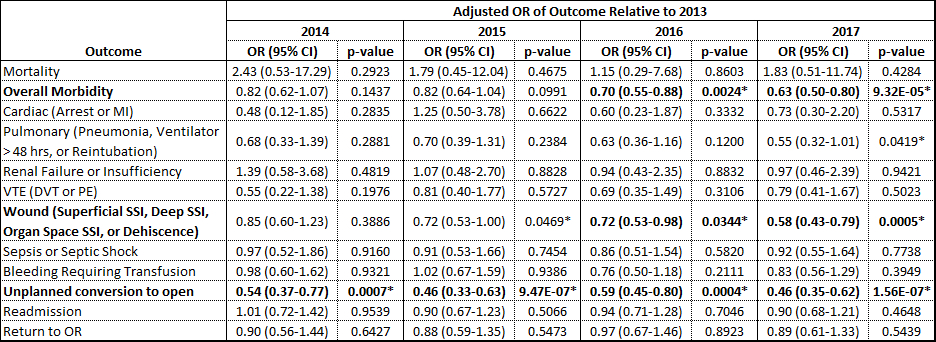
Table 2. Multivariate logistic regression analysis of outcomes by year. *p < 0.05.
Back to 2019 Abstracts




