A NATIONAL DATABASE STUDY ON COLECTOMY AND COLORECTAL CANCER IN ULCERATIVE COLITIS: WHAT IS THE ROLE OF APPENDECTOMY?
Merel E. Stellingwerf*2, Willem A. Bemelman2, Geert R. D'Haens1, Cyriel Ponsioen1, Christianne J. Buskens2
1Department of Gastroenterology and Hepatology, Amsterdam UMC, Amsterdam, Netherlands; 2Department of Surgery, Amsterdam UMC, Amsterdam, Netherlands
Background
Appendectomy prevents the development of ulcerative colitis (UC), and might have a positive effect on the disease course of UC. However, several studies indicated an increased risk of colectomy and colorectal cancer (CRC) after appendectomy in UC, and discourage the use of an experimental appendectomy. Nonetheless, it seems premature to draw strong conclusions, as these retrospective studies did not correct for possible confounding factors. The aim of this study was to evaluate the risk of colectomy and CRC after appendectomy in UC patients, while correcting for relevant confounders.
Methods
All included patients were retrieved from the prospective national inflammatory bowel disease database. From 2007, consecutive IBD patients were continuously invited to participate. For inclusion in the current study, patients had to have UC, and data on both appendectomy and colectomy and/or CRC rate had to be available. Primary outcomes were the risk of colectomy and CRC. Outcomes were compared in patients with and without appendectomy, with a separate analysis for timing of appendectomy (before or after UC diagnosis).
Results
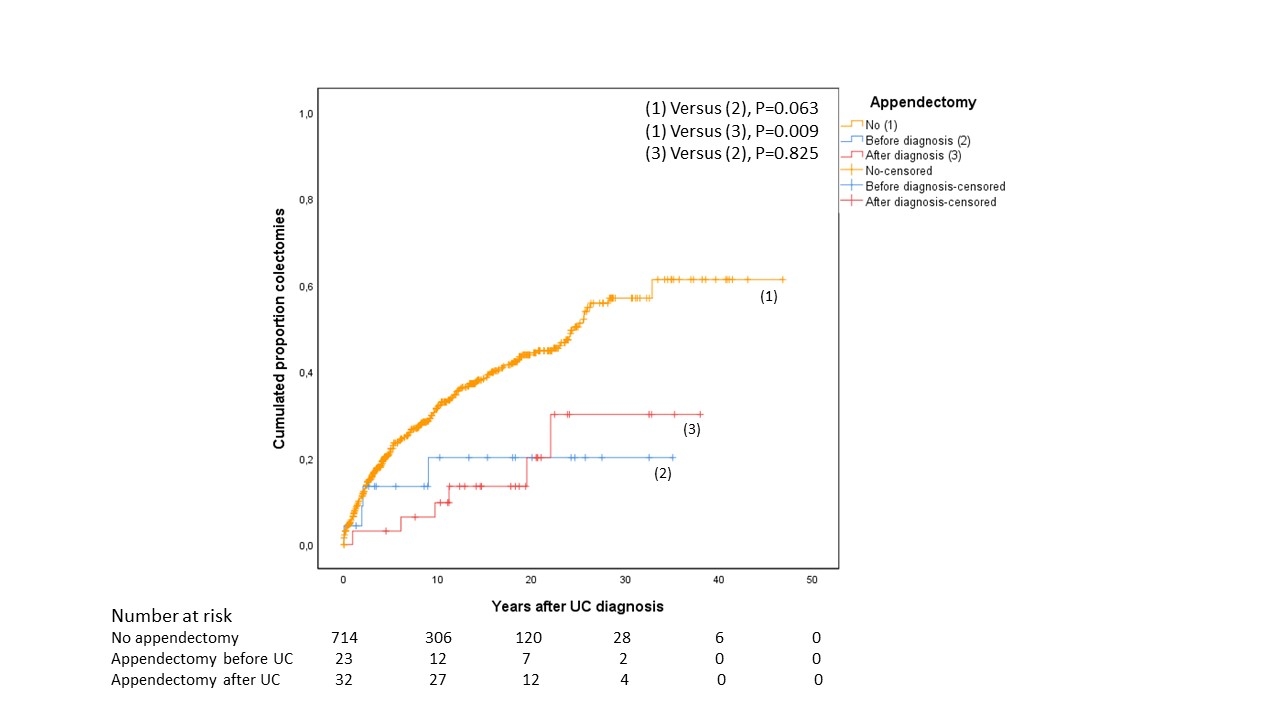
In total, 826 UC patients (54.7% female) with a median age of 46 (range 18-89) years were included from 2007 until May 2018. Sixty-three (7.6%) patients previously had an appendectomy: 24 (38.1%) before UC diagnosis, 33 (52.4%) after diagnosis, and in 6 (9.5%) patients the timing was unknown. On baseline characteristics, patients with an appendectomy had a significantly lower rate of colectomy (19.0% versus 37.6%; P=0.003) and tended to have more often PSC (11.8% versus 5.7%; P=0.090). In multivariate analysis, appendectomy after UC diagnosis was associated with a significantly lower risk of colectomy compared to no appendectomy (HR 0.15, 95% CI 0.04-0.59; P=0.007), and the same trend was seen in patients with appendectomy before UC (HR 0.36, 95% CI 0.09-1.47; P=0.156). Kaplan-Meier analysis demonstrated that appendectomy was associated with a significantly postponed colectomy, in particular when performed after UC diagnosis (P=0.009). No significant differences were found in the CRC rate for patients with and without an appendectomy (1.6% versus 1.2%; P=0.555).
Conclusion
An appendectomy during the course of UC is associated with an 85% decreased risk of colectomy and a postponed resection in patients who did undergo colectomy. As the colon is longer in situ the risk of developing CRC remains, emphasizing the importance of endoscopic surveillance.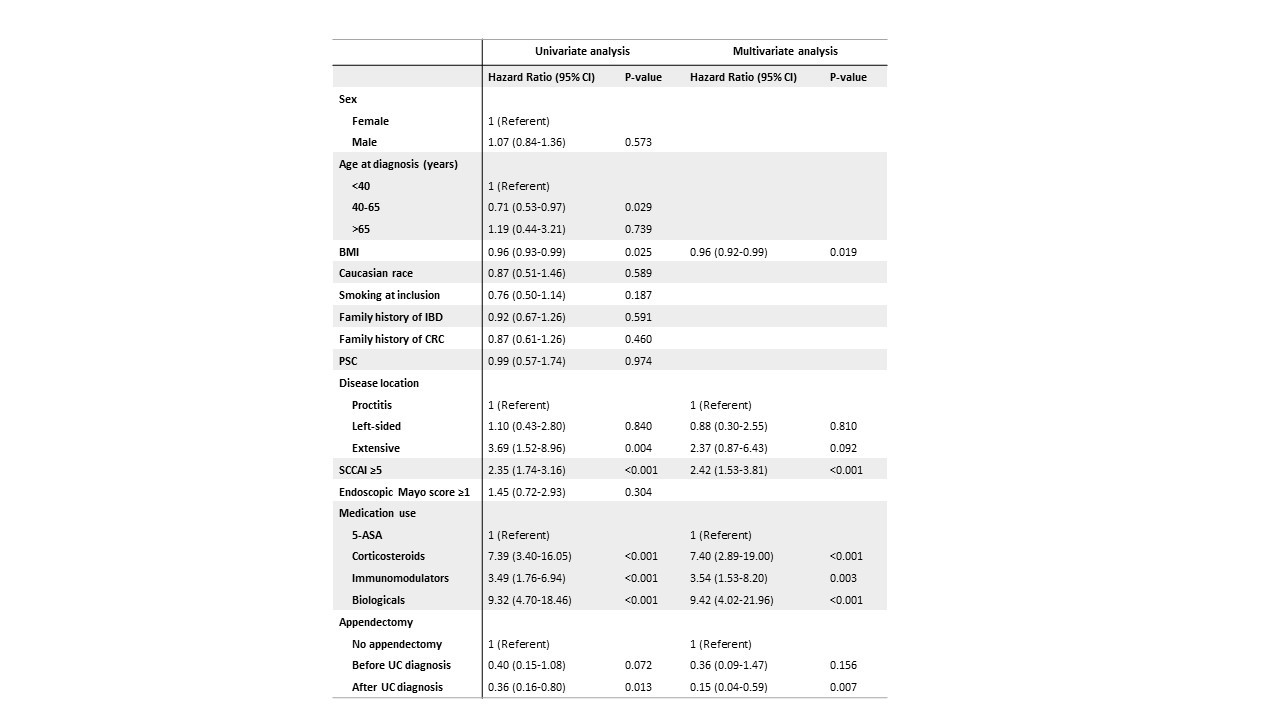
Back to 2019 Abstracts




