ARE ALL MINIMALLY INVASIVE APPROACHES CREATED EQUAL? A COMPARISON OF LAPAROSCOPIC AND ROBOTICS FOR POSTOPERATIVE ILEUS AND QUALITY OUTCOMES IN ELECTIVE COLORECTAL SURGERY
Thais Reif de Paula*1, Samantha K. Nemeth2, James M. Kiely1, Ravi P. Kiran1, Deborah S. Keller1
1Surgery, Division of Colorectal Surgery, Columbia University Medical Center, New York, NY; 2Center for Innovation and Outcomes Rerach, Columbia University Medical Center, New York, NY
BACKGROUND: Postoperative ileus (POI) is a dreaded complication after elective colorectal surgery, with a substantial impact on patient recovery and healthcare utilization. The causes are multifactorial and the most effective intervention to mitigate POI is minimally invasive surgery (MIS). Even with MIS, POI is a common and costly problem. Little study to date was been performed comparing the incidence of POI across MIS platforms. Our goal was to evaluate the prevalence of POI and other 30-day outcomes across the laparoscopic and robotic platforms in elective colorectal surgery.
METHODS: The American College of Surgeons National Surgical Quality Improvement Program (NSQIP) targeted colectomy participant use file was reviewed for elective colorectal resections performed with an MIS approach between 2012 and 2016. Cases were included if they underwent a multiport laparoscopic or robotic assisted laparoscopic approach. Demographic characteristics, operative, and postoperative outcomes were evaluated across groups. The main outcome measure was POI. Secondary outcomes included 30-day major morbidity, surgical site infections (SSI), bleeding, readmissions, reoperations, and hospital length of stay (LOS) between the laparoscopic and robotic approaches. Groups were matched via nearest neighbor Propensity Score Matching (PSM) at a 3:1 ratio. Categorical outcomes were compared using Chi-Squared Test and LOS was evaluated using the Mann-Whitney test. The Holm procedure was used to adjust for multiple endpoints.
RESULTS: 64,194 patients underwent elective colorectal resections during the study period. Of them, 6,837 robotic procedures were matched to 19,670 multiport laparoscopic procedures using nearest neighbor PSM. The incidence of POI was significantly lower in robotic than laparoscopic cases (10.11% vs. 11.54%, p<0.001). Similarly, the occurrence of major morbidity (23.72% vs. 27.68%, p<0.001) and bleeding requiring transfusion (3.95% vs. 5.23%, p<0.001) was lower with robotics. However, there were more unplanned reoperations with the robotic than laparoscopic approach (4.73% vs. 3.92%, p<0.001). The median LOS in both approaches was 4 days. There were no differences in overall SSI (6.91% vs. 7.28%, p=0.381) and readmissions (9.80% vs. 9.23%, p=0.239) between the surgical approaches.
CONCLUSIONS: Elective colorectal resection is an operation with noteworthy risk of ileus complication, which impacts both clinical outcomes and costs. Our study found the MIS approach can make a significant difference in ileus rate. Robotic colorectal resections had fewer ileus complications and decreased major morbidity than laparoscopic cases. With the transition to value-based care, the improved outcome metrics with robotics could show a unique value proposition for this MIS approach in colorectal surgery.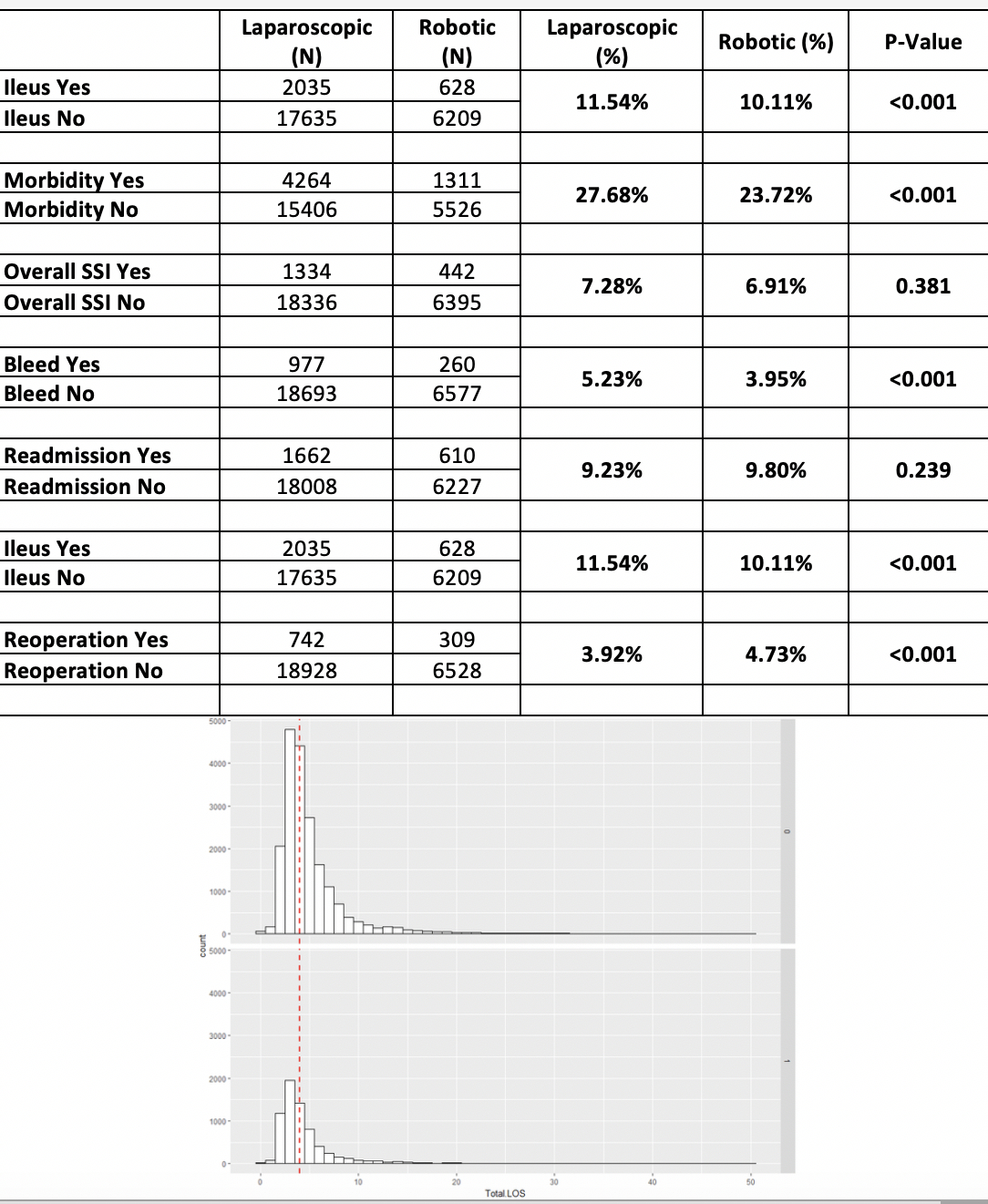
Back to 2019 Abstracts




