LAPAROSCOPIC PARTIAL COLECTOMY IS THE MOST COST EFFECTIVE SURGICAL APPROACH TO PATIENTS WITH COLON CANCER
Emanuel Eguia*1, Patrick Sweigert1, Joshua Eberhardt1, Marc Singer1, Majid Afshar1, PAUL KUO2, Marshall S. Baker1
1Surgery, Loyola University Medical Center, Maywood, IL; 2Surgery, University of Southern Florida, Tampa, IL
BACKGROUND
The use of robotic-assisted partial colectomy (RC) is becoming more commonly applied to patients with colon cancer. Few studies compare short- and long-term outcomes and aggregate costs associated with RC and laparoscopic (LC) or open (OC) partial colectomy.
METHODS
We queried the Healthcare Cost and Utilization Project State Inpatient Database to identify patients with colon cancer undergoing elective colectomy in FL, IA, MA, WI, MD, NY, and WA between 2013 and 2014. Multivariable regression (MVR) was used to evaluate the association between surgical approach (OC vs. LC vs. RC) and rates of postoperative complication, overall lengths of stay (LOS), and aggregate costs of care including readmissions to 90 days following the index procedure. Candidate variables for analysis were determined a priori using best variable subsets. MVR models were adjusted for age, gender, Charlson Co-morbidity Index (CCI), hospital colectomy volume, insurance, and procedure type. Hospital volume for colectomy was broken to terciles (low: <73 colectomies/year; moderate: 73-155 colectomies/year; high volume: 155 colectomies/year).
RESULTS
11,111 patients underwent LC (58%), 262 RC (1.4%) and 7,610 OC (40%). On univariate analysis, patients undergoing partial LC and RC were more likely to be white (79% vs. 66%; p<.01), have Medicare insurance (58% vs. 67%; p<.01), and undergo right colectomy (77% vs. 76%; p<.01). Patients undergoing LC were less likely than those undergoing RC to have a 90-day readmission (12% vs. 13%; p<.01), in-hospital mortality (0.5% vs. 1.9%; p<.01) and had lower overall costs ($14,500 vs. $17,000).
On MVR, LC was associated with a lower odds risk than both RC and OC of having any overall complication (OR 0.51; 95% CI 0.36, 0.71]; OR 0.57; 95% CI 0.52, 0.62]), in-hospital mortality (OR 0.25; 95% CI [0.10, 0.65]; OR 0.54; 95% CI [0.38, 0.75]), prolonged LOS (OR 0.57; 95% CI [0.36, 0.91]; OR 0.50; 95% CI [0.45, 0.57]), and of being a high cost outlier (OR 0.47; 95% CI [0.34, 0.65]; OR 0.60; 95% CI [0.55, 0.66]). (Table 1)
In moderate and low volume centers, LC was also associated with lower aggregate risk-adjusted costs relative to both RC and OC (-$5,383; 95% CI [-$9,264, -$1,502]; -$3,965; 95% CI [-$5,302, -$2,897]). In high volume centers, costs of LC, RC and OC were statistically identical.
CONCLUSION
In patients undergoing elective surgery for colon cancer, LC is associated with lower rates of postoperative complication, decreased LOS and lower rates of in-hospital mortality compared to either RC or OC. These results translate to lower aggregated costs in moderate volume centers and a lower likelihood of being a high-cost outlier independent of hospital volume. These findings suggest that LC is a safer and more cost-effective surgical approach to colon cancer than either OC or RC.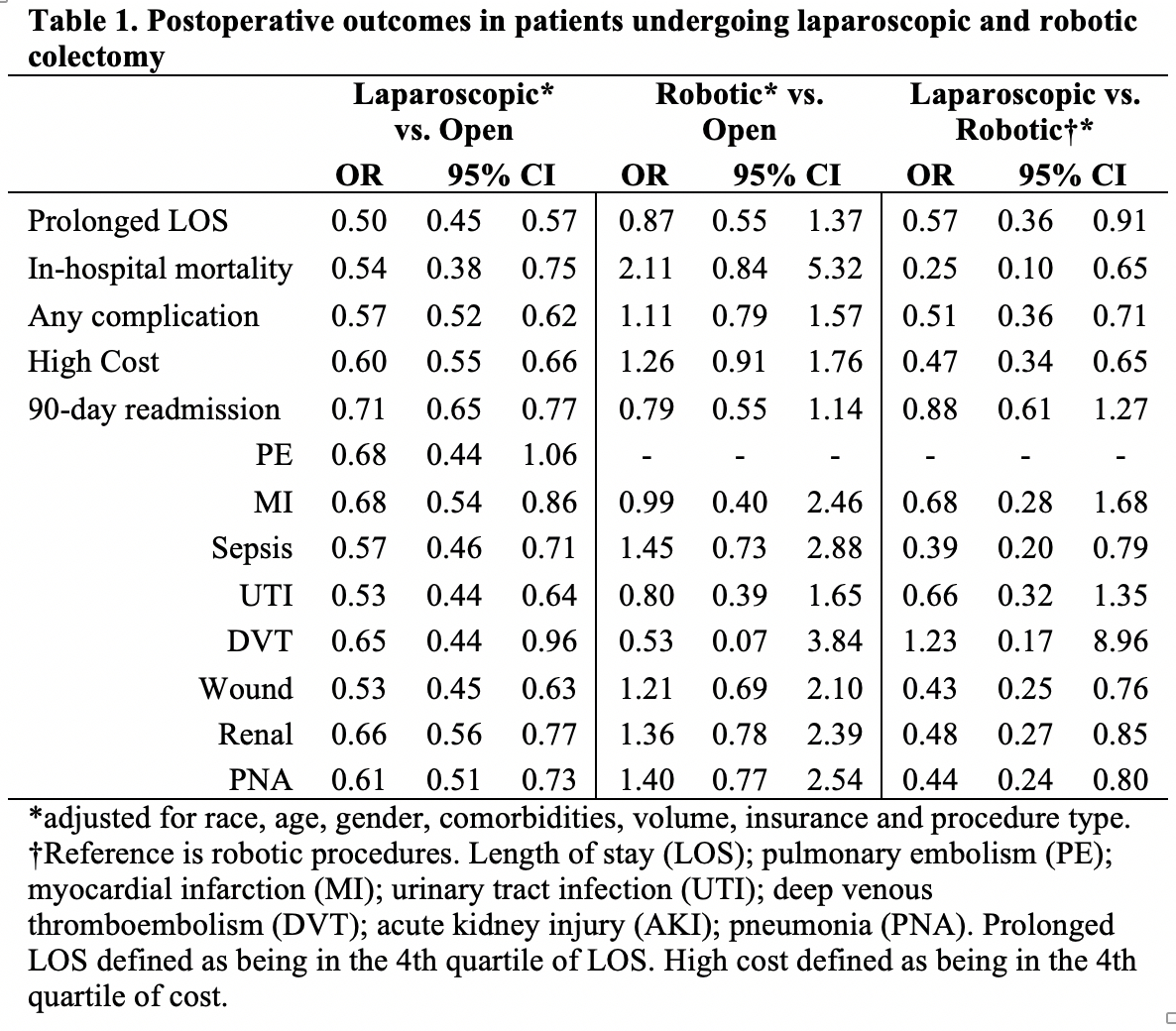
Back to 2019 Abstracts




