DECLINE IN UNNECESSARY SURGERY FOR LOCALLY ADVANCED RECTAL CANCER DUE TO ADEQUATE MULTIDISCIPLINARY RESPONSE EVALUATION FOLLOWING CHEMO-RADIOTHERAPY
Jelle F. Huisman*1, Ivonne Schoenaker1, Richard Brohet2, Onne Reerink3, Hedwig van der Sluis1, Freek Moll4, Erwin de Boer5, Jacques de Graaf6, Wouter de Vos tot Nederveen Cappel1, Erik van Westreenen7
1Gastroenterology, Isala, Zwolle, Overijssel, Netherlands; 2Epidemiology and statistics, Isala, Zwolle, Netherlands; 3Radiotherapy, Isala, Zwolle, Netherlands; 4Pathology, Isala, Zwolle, Netherlands; 5Radiology, Isala, Zwolle, Netherlands; 6Oncology, Isala, Zwolle, Netherlands; 7Surgery, Isala, Zwolle, Netherlands
BACKGROUND: Standard therapy for locally advanced rectal cancer is neoadjuvant chemo-radiation therapy (nCRT) to downstage the tumor followed by total mesorectal excision (TME). Pathologic Complete Response (pCR) after nCRT was found in 25% of these carcinomas. Therefore, a so called wait and see (W&S) strategy has been introduced as an alternative therapy. Selected patients with clinical Complete Response (cCR) during restaging with endoscopy and MRI might benefit from organ sparing therapy. Aim of our study was to compare the proportion of patients with pCR since the introduction of the multidisciplinary response evaluation (MRE) in our hospital with the period before structural response evaluation.
METHODS: In this retrospective cohort study, patient with locally advanced rectal cancer (tumor stage T3 or T4 with threatened or involved Mesorectal fascia (MRF) and/or more than three suspected locoregional lymphnodes) who underwent nCRT between 1 January 2009 and 31 May 2018 were included. Patients without MRE were categorized in cohort A. Patient who underwent MRE, introduced in 2015, with endoscopy and diffusion weighted (DWI) MRI were categorized in cohort B. Patients with cCR during restaging were offered a W&S strategy. pCR was defined as ypT0N0
RESULTS: A total of 263 patients were included in the study, 128 in cohort A and 135 in cohort B (Figure 1). In cohort A, 114 patients (89%) underwent TME after a median of 10 [5-29] months. pCR was found in 21 patients (16.4%). In cohort B, 40 patients (30%) underwent W&S, 83 patients (61%) underwent primary TME after a median of 15 [10-44] weeks and 7 patient underwent TME due to local regrowth during W&S. pCR was found in 8 patients (5.9%) in cohort B, which was significant lower than in cohort A (p=0.007). Local regrowth during W&S was found in 10 patients (25%) after a median of 14 [7-24] months. Nine of these patients underwent curative salvage surgery (TME or TEM), the other patient developed distant metastasis and underwent palliative therapy.
CONCLUSION: MRE after nCRT has led to a significant decrease in unnecessary surgery in patients with locally advanced rectal cancer.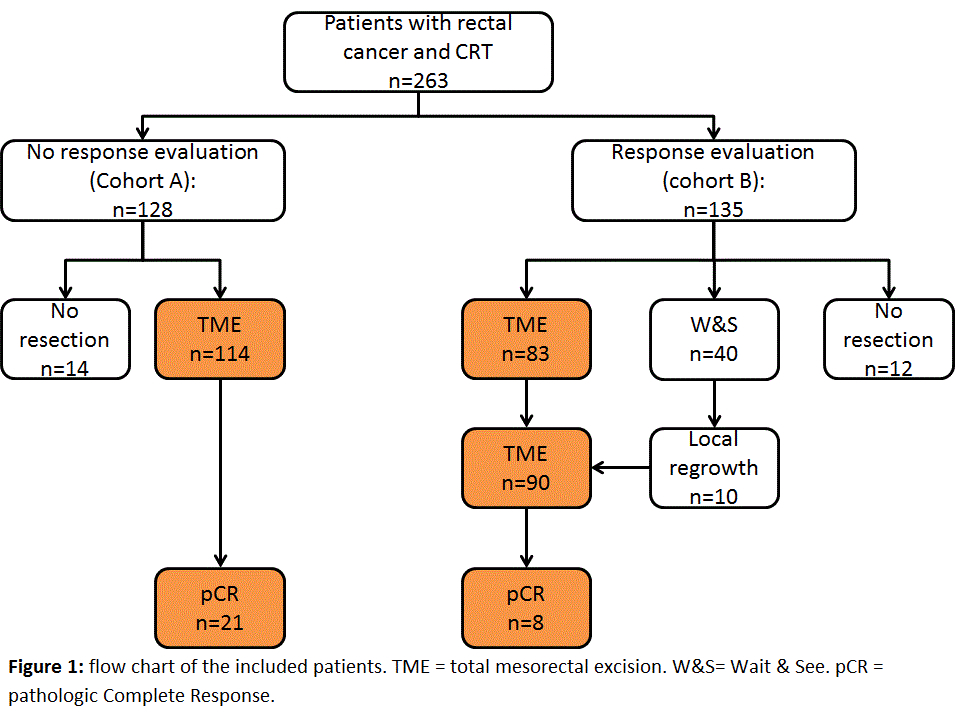
Back to 2019 Abstracts




