BARRETT'S ESOPHAGUS IS A LONG-TERM COMPLICATION OF SLEEVE GASTRECTOMY: A SYSTEMATIC REVIEW AND META-ANALYSIS
Nicholas A. Hoerter*, Scott M. Smukalla, Max Pitman, Violeta Popov
New York University Langone Health, New York, NY
Laparoscopic sleeve gastrectomy (LSG) has rapidly risen in popularity to become the most common bariatric procedures in the US, accounting for 58% of procedures in 2016, up over 300% since 2011. Accordingly, short-term complications are well-studied but long-term data has only recently become available. Some studies suggest increased gastroesophageal reflux, esophagitis, and Barrett's esophagus (BE) after LSG.
Aim: The aim of the current study is to systematically review and analyze the literature to assess the incidence of BE after LSG by comparing patients' pre- and post-operative endoscopic findings.
Methods: MEDLINE and Embase were searched through August 2018 with the mesh terms "?endoscopy"?, "bariatric surgery"?, "Barrett's esophagus"?, "sleeve gastrectomy"?. Selection of studies and extraction of data were performed independently by two authors. Inclusion criteria were retrospective and prospective studies reporting endoscopic outcomes both before and after LSG. The primary outcome was the incidence of BE after LSG summarized with odds ratio (OR) and 95% confidence interval (CI) compared to pre-LSG and event rates in a random-effects model. Subgroup analyses by duration of follow-up (<24 months or >24 months) and by removing studies that excluded patients with endoscopic findings pre-operatively were performed. Secondary outcomes included event rates and ORs of hiatal hernia, esophagitis, and GERD symptoms after LSG.
Results: 1422 citations were identified; 95 studies were reviewed by full text, and two study authors were contacted for additional information. 8 prospective and 1 retrospective study including 968 subjects were analyzed. The average follow-up was 29 months (range 2 months to 11 years), average age 37.8 years, with 73% female. The OR for BE after LSG was 7.44 (95% CI 2.25-24.66, I2=0.0), Figure 1. Overall BE developed after LSG in 3.4% of patients (event rate 0.034, 95% CI 0.011-0.099, I2=84.3%). Notably, BE incidence was significantly higher in studies with longer follow-up, with an event rate of 13.3% in studies with >24 months follow-up, compared to 1.4% in studies with <24 months follow-up (p value <0.005), Figure 2. New-onset esophagitis was seen in 22.6% (95% CI 14.7-32.9%, I2=88.0%) of patients. The OR for esophagitis was 5.76 (95% CI 2.79-11.91, I2=69.8%), for hiatal hernia 3.41 (95% CI 1.08-10.75, I2=54.5%), and for GERD 4.78 (95% CI 1.94-11.81, I2=81.4%). The ORs for these findings remained significantly higher even after removing studies that excluded subjects with esophageal abnormalities preoperatively.
Conclusion: LSG increases the risk of developing BE and the effect is more pronounced with time, as would be expected based on the pathophysiology of Barrett's. Related complications include GERD, esophagitis, and hiatal hernia. These results suggest that a screening protocol for BE in LSG patients may be beneficial.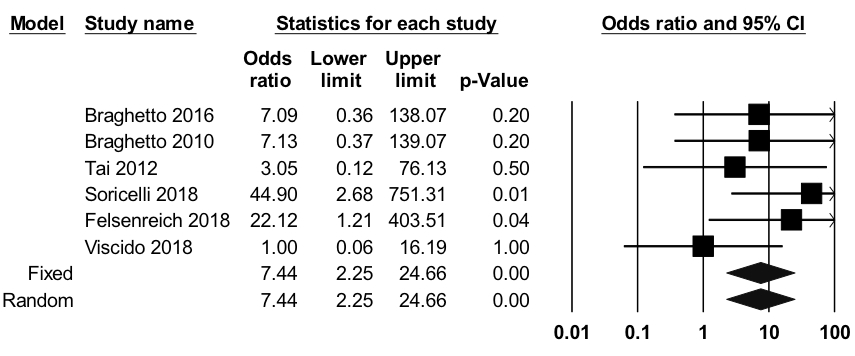
Figure 1. Odds Ratio for Barrett's esophagus after laparoscopic sleeve gastrectomy including six individual studies and the pooled rate, with Forest plot. N=782, I2=0.0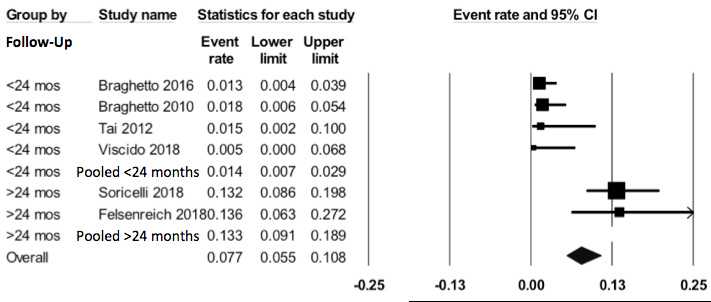
Figure 2. Subgroup analysis showing event rates for Barrett's esophagus after laparoscopic sleeve gastrectomy with studies grouped by length of follow up after surgery, with Forest plot. N=782 p<0.005
Back to 2019 Abstracts




