SHOULD DIFFUSE MAIN-DUCT INTRADUCTAL PAPILLARY MUCINOUS NEOPLASMS BE TREATED WITH TOTAL PANCREATECTOMY?
Alex Blair*, Ross M. Beckman, James F. Griffin, Vincent P. Groot, Jun Yu, Martin Makary, Richard Burkhart, Matthew J. Weiss, John Cameron, Christopher L. Wolfgang, Jin He
Surgery, Johns Hopkins Hospital, Baltimore, MD
Background: Main-duct (MD) intraductal papillary mucinous neoplasm (IPMN) is associated with a high risk of malignancy. There is a lack of international consensus (partial or total pancreatectomy) when the MD of the whole gland is involved. The fate of the remnant after partial pancreatectomy for benign diffuse MD-IPMN is unclear.
Methods: Consecutive patients with partial pancreatectomy for benign MD-IPMN from 2004 to 2016 were analyzed. Exclusion criteria include any malignancy on final pathology and less than one year of post-operative follow-up. Diffuse MD-IPMN was defined by preoperative imaging as dilation of the MD in the head of the pancreas more than 5mm and involving the whole gland.
Results: Of 127 patients with resected benign MD-IPMN, 47 (37%) had diffuse MD involvement. The majority (96%) underwent pancreaticoduodenectomy and 2 (4%) had distal pancreatectomy secondary to a cyst or larger MD dilatation in the tail. Median age was 73 (IQR: 67-79) with median duct size of 8 mm (IQR 6-13mm). High grade dysplasia (HGD) was observed in 24 (51%), intermediate grade in 21 (45%) and low grade in 2 patients (4%). Two patients had HGD at the resection margin. A median progression free survival (PFS) of 84 months was observed, with 10 (22%) patients developing imaging evidence of progression or new cystic disease in the pancreatic remnant at a median of 25 months. Three of 10 (30%) underwent completion pancreatectomy with no cancer identified in the remnant. A margin positive with intermediate or high grade dysplasia was significantly associated with shorter PFS (HR:4.39, 95%CI 1.05-18.46, p=0.043). When compared to those with focal MD involvement, patients with diffuse MD-IPMN were older (73 vs 67, p=0.009), more likely to receive a pancreaticoduodenectomy (96% vs 56%, p<0.001) and more likely to have high grade dysplasia (51% vs 31%, p=0.025). Nevertheless, MD involvmenet (diffuse vs focal) was not associated with PFS following surgery (p=0.328).
Conclusions: Partial pancreatectomy is an appropriate surgical approach for diffuse MD-IPMN and is not associated with earlier progression after surgery. Progression in the pancreatic remnant requires ongoing close follow-up.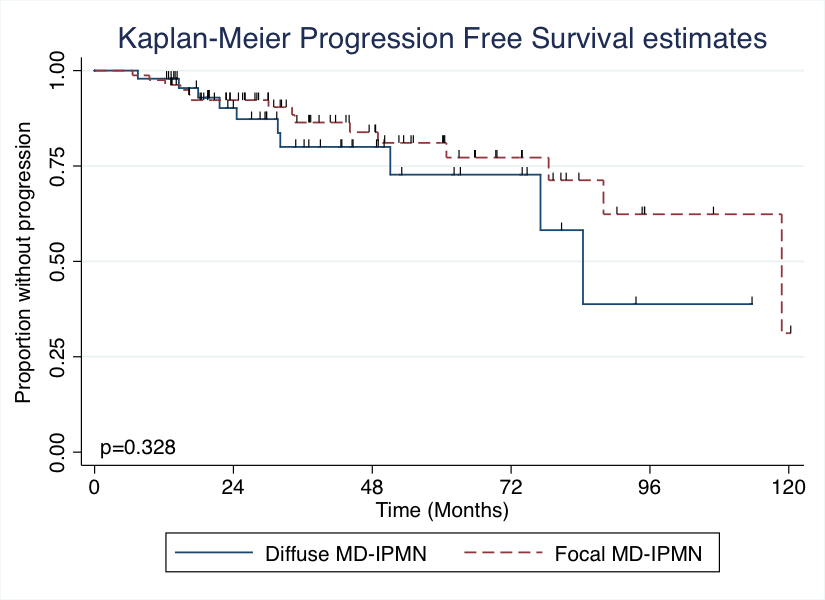
Figure 1.The degree of main duct involvement, diffuse vs focal, was not associated with a shorter progression free interval in patients with partial pancreatectomy for benign IPMN.
Back to 2019 Abstracts




