IS BARIATRIC SURGERY SAFE AND EFFECTIVE IN PATIENTS WITH INFLAMMATORY BOWEL DISEASE? A MULTI-INSTITUTIONAL EXPERIENCE
Nicholas P. McKenna, Elizabeth B. Habermann, Alaa Sada*, Todd A. Kellogg, Travis J. McKenzie
Surgery, Mayo Clinic, Rochester, MN
BACKGROUND: Twelve percent of patients with inflammatory bowel disease (IBD) have either serious or severe obesity, but the safety and efficacy of bariatric surgery in patients with IBD is not fully understood. Our aim was to evaluate the short and long-term safety and efficacy of bariatric surgery in patients with IBD.
METHODS: A retrospective review was conducted of patients undergoing bariatric surgery with a preoperative or postoperative diagnosis of IBD across three academic centers between August 2006 and December 2017. Data was collected on IBD characteristics and medications, postoperative complications, the need for future IBD-related surgery, and weight loss at 6, 12, and 24 months.
RESULTS: Thirty-three patients with a median age of 51 years (range, 32-60) and median duration of IBD of 13 years (range, 3-43) underwent 34 bariatric operations. A Roux-en-Y gastric bypass [RYGB] was performed in 16 patients (N=9 ulcerative colitis [UC], 6 Crohn's disease [CD], 1 IBD indeterminate), a sleeve gastrectomy [SG] in 14 patients (N=7 UC, 7 CD), and a gastric band in 4 patients (N=4 UC). Mean (±SD) BMI of the cohort before intervention was 42.7 (±4.9). Thirty-one patients had an existing diagnosis of IBD, and two were diagnosed with CD after RYGB. Nine patients were on preoperative immunosuppression (N=4 biologics, 3 immunomodulators, 2 corticosteroids) for IBD, and 11 had undergone prior intestinal resection for IBD.
Average hospitalization for the entire cohort was 3.6 days and four 30-day infectious complications were observed (N=2 superficial surgical site infections, 1 infected intra-abdominal hematoma, 1 hepatic abscess). Long-term, reoperation was required for failed gastric band (N=3), reduction of internal hernia (N=2) and cholelithiasis (N=2). The mean (±SD) percentage of overall excess weight loss was 57.5% (±24.8) at 6 months, 63.3% (±33.1) at 12 months, and 58.6% (±26.6) at 24 months (FIGURE). At a mean follow-up of 3.4 years, there were no IBD flares requiring surgery.
CONCLUSION: In highly selected patients with well-controlled IBD, bariatric surgery results in sustained weight loss over a two-year period. While both SG and RYGB appear safe in patients with either UC or CD within this cohort, caution should be still be exercised before performing a RYGB in a patient with CD. Increased utilization of bariatric surgery may help mitigate the obesity epidemic that is ongoing within this patient population.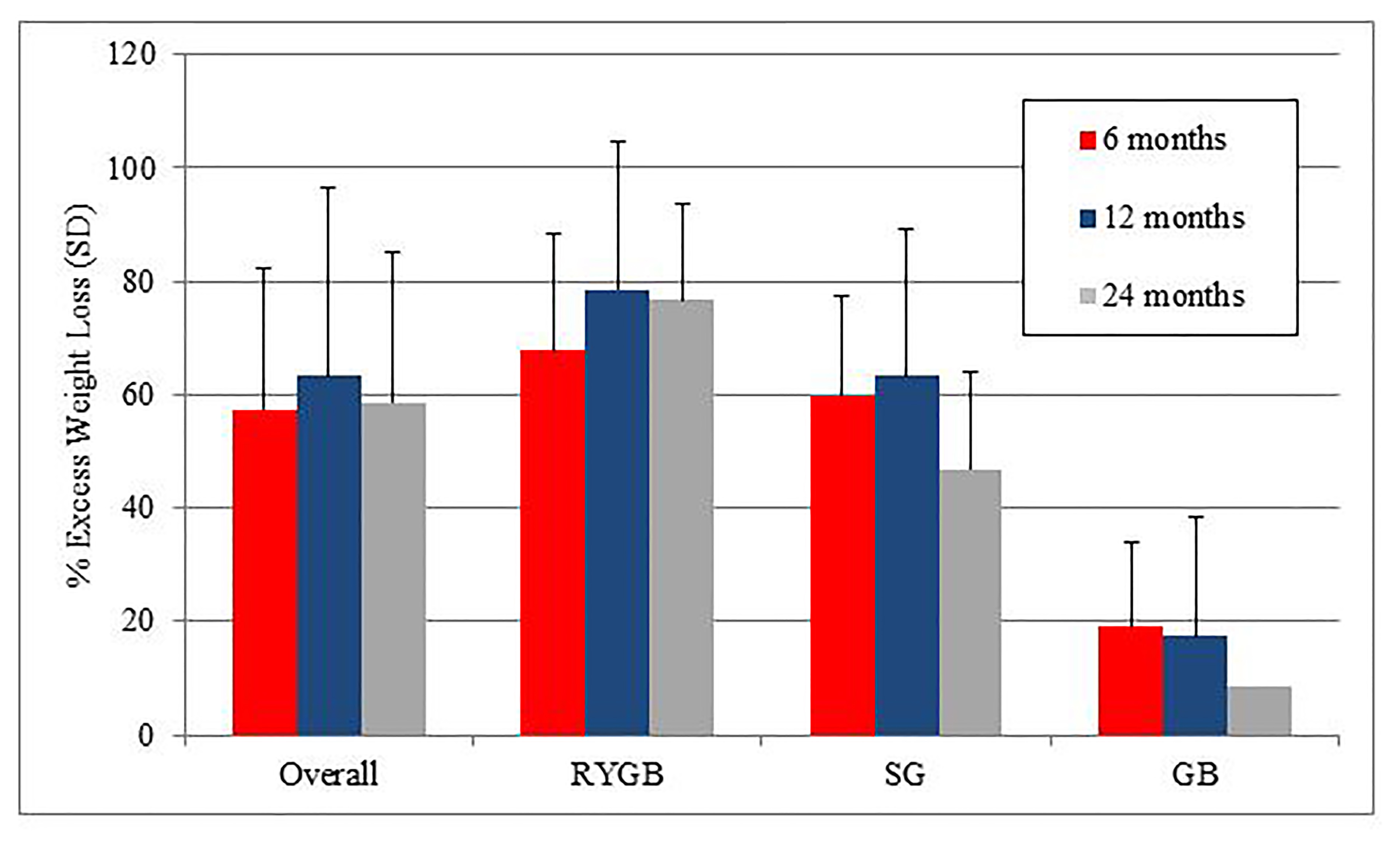
FIGURE. Mean percentage of excess weight loss overall and across the three operations. RYGB: Roux-en-Y Gastric Bypass; SG: Sleeve Gastrectomy; GB: Gastric Band
Back to 2019 Abstracts




