CLINIC-BASED SCREENING AND DETECTION OF PHYSICAL FRAILTY AND NEUROCOGNITIVE DYSFUNCTION IN PATIENTS UNDERGOING ONCOLOGIC LIVER RESECTION
Heather A. Lillemoe*, Rebecca K. Marcus, Bradford J. Kim, Nisha Narula, Catherine H. Davis, Thomas Aloia
Department of Surgical Oncology, University of Texas MD Anderson Cancer Center, Houston, TX
Background: Frailty is a risk factor for adverse outcomes and delayed recovery after surgery. Its impact can affect survival in cancer patients, who depend on recovery in order to rapidly return to other oncologic therapies. However, the practicing surgeon rarely screens for frailty.
Objectives: To address this knowledge gap, this pilot study was designed to assess the feasibility of administering a clinic-based battery of validated tools to characterize the incidence of physical frailty and neurocognitive dysfunction in patients undergoing hepatectomy.
Methods: Adult patients undergoing hepatectomy from Oct. 2017 through Sept. 2018 were prospectively evaluated for physical frailty and neurocognitive dysfunction before and after their operation (Figure 1). Physical tests included the grip strength (GS) and "Timed Up and Go"? (TUG) tests. Neurocognitive function was evaluated with the Mini-Cog test. To identify symptom burden, the M.D. Anderson Symptom Inventory (MDASI-GI) patient-reported outcome (PRO) measure was used. ECOG performance status was also captured.
Results: The median patient age was 64 years and 56% of patients received preoperative chemotherapy. The median duration of testing was 7.5 minutes (maximum duration: 10 minutes). On preoperative assessment, deficits were identified in 7/25 patients (28%) based on GS, 1/25 patients (4%) based on TUG, and 3/25 patients (12%) based on Mini-Cog. Three patients (12%) screened positive in more than one category. Despite 7 patients (28%) having a severe preoperative symptom burden on PRO, only one patient rated an ECOG >1. For patients whose first postoperative evaluation was within 2 weeks of surgery (n=17), recovery to or above baseline was present for 11/14 (79%) based on GS, 5/17 (29%) based on TUG, and 11/17 (65%) based on Mini-Cog. Six patients' (35%) ECOG returned to baseline (or better). Two patients were completely recovered across all measures. For patients whose first postoperative evaluation was >2 weeks from surgery (n=8), 2/8 (25%) were recovered based on GS, 4/8 (50%) based on TUG, and 7/8 (88%) based on Mini-Cog. Four patients' (50%) ECOG returned to baseline (or better). Two patients were completely recovered. Overall, 12/25 (48%) patients returned to baseline (or better) symptom burden at first follow-up.
Conclusions: This study reports the feasibility of a quick and easy-to-use battery of tests for assessing frailty and recovery. For cancer surgery patients, this clinic-based assessment appears to be more granular and more sensitive than the commonly reported ECOG. Use of this approach could trigger necessary preoperative supportive or geriatric assessment to better optimize at-risk patients. Future efforts are aimed at correlating frailty to longer-term outcomes and developing a cohesive frailty score to be validated within a larger patient group.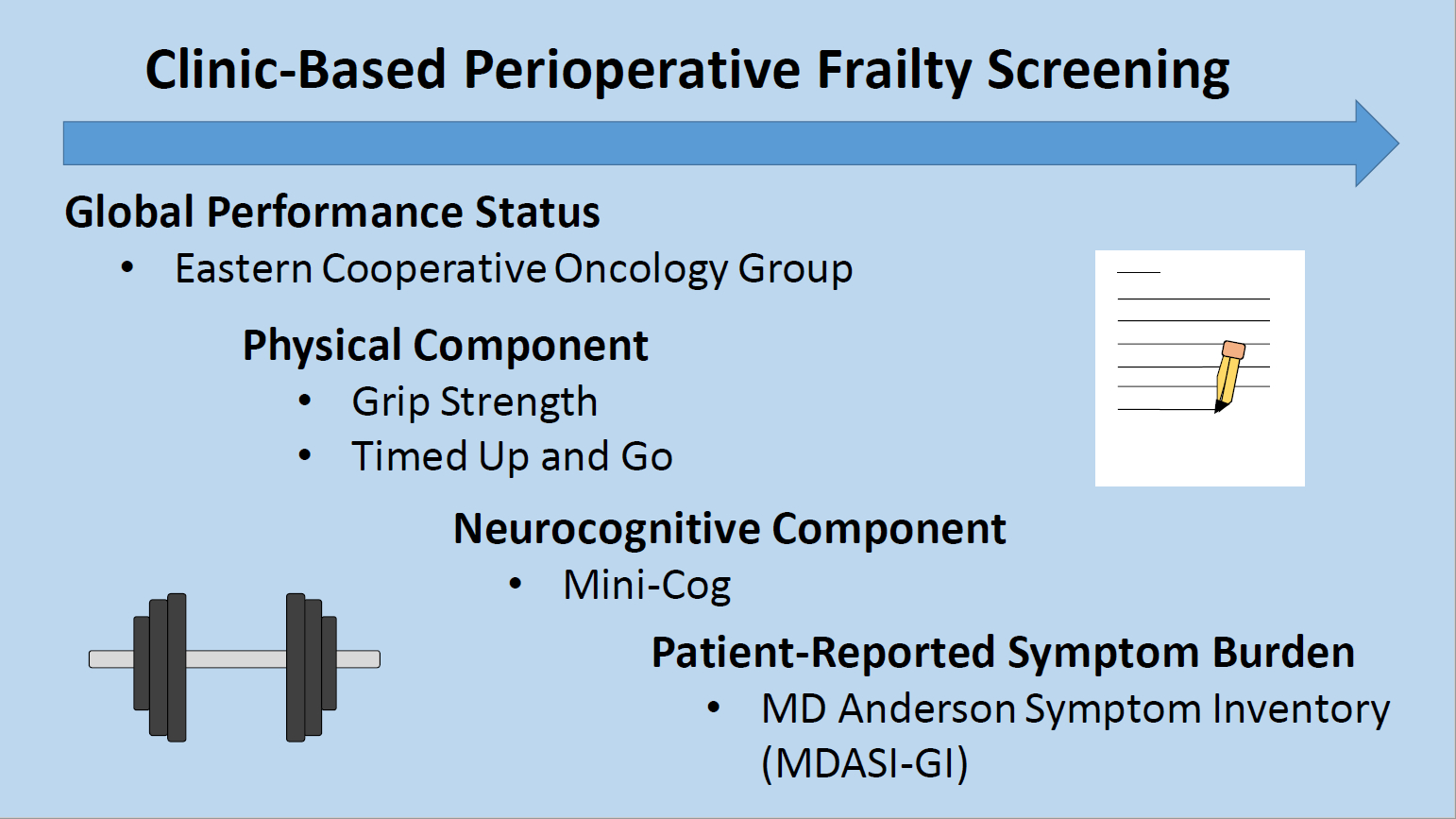
Back to 2019 Abstracts




