DOES FUNDOPLICATION IMPROVE THE LONG-TERM RESULTS OF LAPAROSCOPIC HELLER MYOTOMY
Christina L. Costantino*1, Abraham D. Geller1,2, Micheal R. Visenio3,1, Christopher R. Morse1, David W. Rattner1
1Surgery, Massachusetts General Hospital, Boston, MA; 2Harvard Medical School, Boston, MA; 3Harvard T.H. Chan School of Public Health, Boston, MA
Introduction: Most published reports of Laparoscopic Heller Myotomy (LHM) contain only short-term follow up, but the few series with long-term follow up suggest that peptic damage is a major cause of late failure following LHM. A major concern about widespread adoption of POEM as a replacement for LHM is the documented pathologic acid exposure rates in approximately 50% of patients following POEM. Therefore, we reviewed our experience with LHM to determine both the long-term success rate, as well as patterns of failure following LHM in patients with and without fundoplications.
Methods: A single institution, prospectively maintained database of patients undergoing foregut surgery was queried to identify patients undergoing LHM between 1995 - 2017. Eckardt scores (ES) were obtained by patient's responses to an IRB approved questionnaire at three time points 1) prior to LHM (baseline), 2) 1-year following LHM, and 3) within the past year. Additional data were gathered by chart review. Primary outcome measure was treatment success defined as ES of <3. Secondary endpoints were durability of symptomatic relief and need for reintervention.
Results: Completed surveys were returned by 130 patients with a median follow-up of 8.6 years. Median age at time of operation was 50 (range 18-83) and 58/130 (44.6%) patients were female. Toupet fundoplication was performed at the time of LHM in 63% (n=82) of patients. At both 1-year and late follow-up, patients reported a significant improvement in ES compared to baseline (median decrease of ES from 8 to 2, p<0.05). In the cohort of 44 patients followed for ≥10 years, 37 patients (82%) reported ES <3 at 1 year (P<.001), and 35 patients (78%) at time of last follow-up (P<.001). Of all patients who reported ES <3 at one year post LHM (103/130), 85% continued to report symptomatic relief at last follow-up (median follow-up of 6.9 years in this subgroup). Cohort analysis by 5-year cohorts did not show deterioration of dysphagia relief over time (Fig. 1). The presence or type of fundoplication had no impact on the durability of symptom relief or need for reintervention. Those patients requiring reintervention (n=19) following LHM, underwent dilation (n=17) or botox (n=2) at a median of 3.3 years (range 0.30-17.1 years) after LHM for symptomatic relief. No patients in this cohort required esophagectomy following LHM.
Conclusions: This study is one of the few to report very long-term follow up of LHM and demonstrates that LHM provides immediate and durable long-term symptomatic relief of dysphagia. The addition of fundoplication to LHM neither impacted the durability of dysphagia relief, nor the need for reintervention. Very few patients undergoing LHM in expert hands require further therapeutic intervention. For a majority of patients, treatment success at 1-year is predictive of long-lasting symptomatic relief.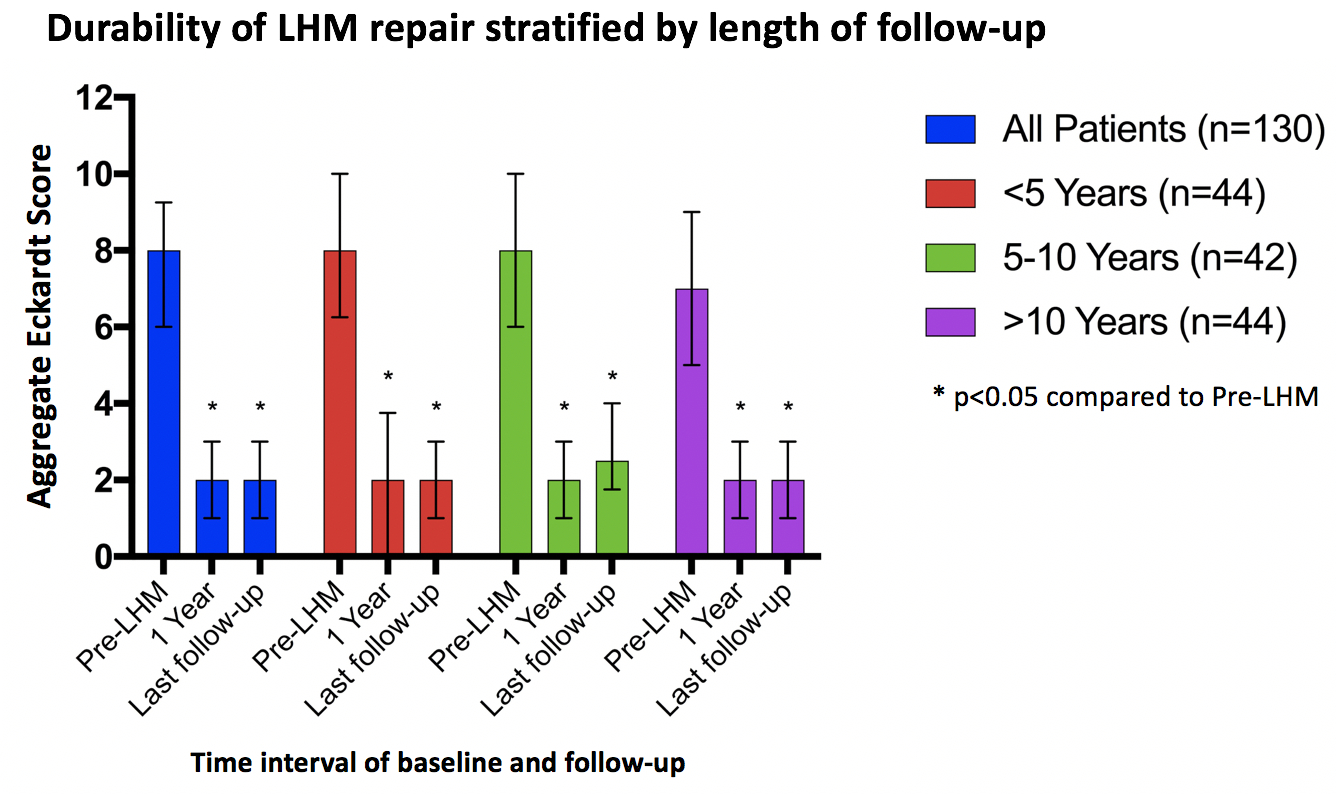
Figure 1. Durability of LHM repair stratified by length of follow-up
Back to 2019 Abstracts




