MINIMALLY INVASIVE SURGERY IS ASSOCIATED WITH INCREASED USE OF POSTOPERATIVE CHEMOTHERAPY FOR LOCALLY ADVANCED GASTRIC CANCER
Rhami Khorfan*1, Cary Jo Schlick1, David J. Bentrem2, Ryan P. Merkow1
1Surgical Outcomes and Quality Improvement, Northwestern University, Chicago, IL; 2Department of Surgery, Northwestern University, Chicago, IL
Objective
Minimally invasive surgery (MIS), including laparoscopic and robotic techniques, is increasingly used in the treatment of gastric cancer in the United States. Previous small series have suggested that patients who undergo MIS may be more likely to receive indicated postoperative chemotherapy. However, the association between MIS and the receipt of appropriate perioperative chemotherapy on a national scale is unknown. Our objectives were (1) to assess trends and predictors of MIS for gastric cancer, and (2) to evaluate its association with the use of postoperative chemotherapy.
Methods
Patients with gastric adenocarcinoma were identified in the National Cancer Database from 2010-2015. Only patients without metastatic disease treated surgically for T3 or greater and/or N+ disease were included in the analysis. Patients over the age of 85, and those who had exceptions to receiving chemotherapy such as severe co-morbidities, refusal, or death were excluded. Patients who received only preoperative chemotherapy were also excluded. The association between operative approach and postoperative chemotherapy (either with or without neoadjuvant therapy) was assessed with hierarchical multivariable logistic regression, adjusting for patient, oncologic, and hospital factors.
Results
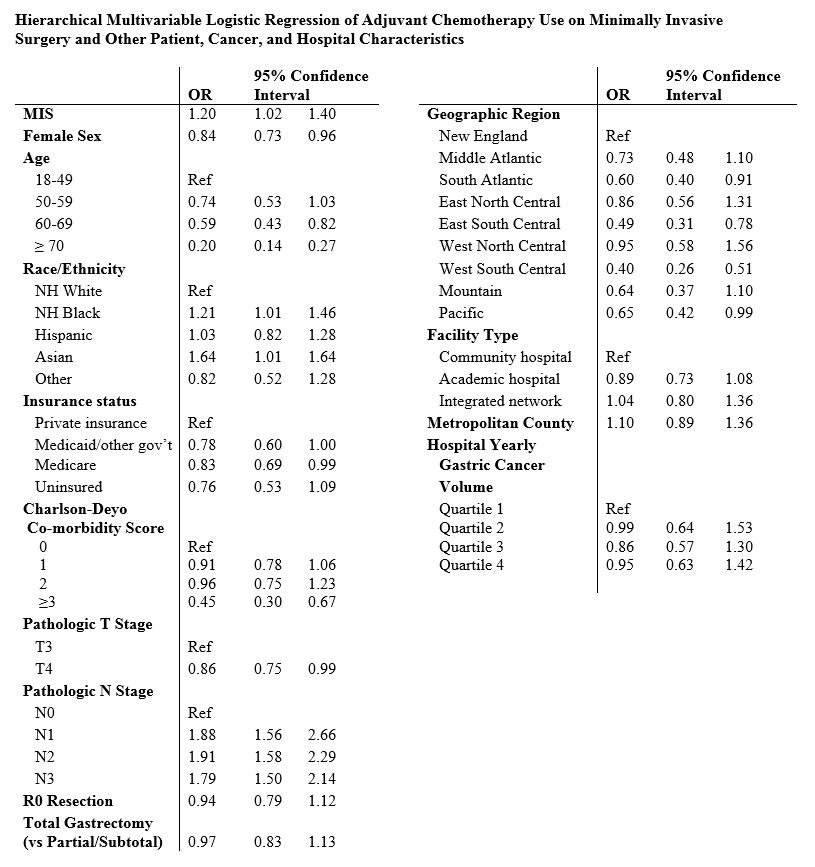
Of the 6,038 patients who underwent surgery for gastric adenocarcinoma, 1,401 (23.2%) underwent MIS and 4,637 (76.8%) underwent open surgery. Of those, 4,119 (24.0% MIS) were partial/subtotal gastrectomy and 1,499 (21.5% MIS) were total gastrectomy. Overall, the proportion of gastric cancers treated with MIS has steadily increased from 16.9% in 2010 to 35.0% in 2015 (Figure, p<0.01). Predictors of MIS approach were any insurance coverage (vs. none), N+ disease, and high hospital gastric cancer volume (vs. low volume). Overall, 4,800 (69.8%) patients received postoperative chemotherapy. MIS was significantly associated with the use of postoperative chemotherapy (with or without neoadjuvant) compared to open surgery (64.8% open vs 70.1% MIS; OR 1.20, 95% CI 1.02-1.40). Other factors significantly associated with postoperative chemotherapy use included male sex, younger age, non-white race, lower Charlson-Deyo co-morbidity score, T3 (vs. T4) tumor, and lymph node involvement (Table).
Conclusion
The use of MIS for gastric cancer increased nearly 2-fold during the study period and is associated with several patient, tumor, and hospital specific factors. Compared to open surgery, patients who underwent MIS for locally advanced gastric adenocarcinoma were more likely to receive postoperative chemotherapy.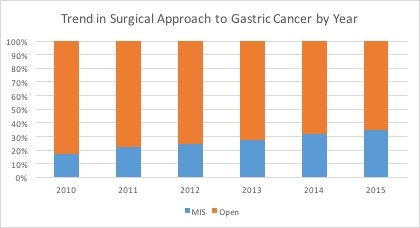
Back to 2019 Abstracts




