INFLUENCE OF EARLY CHOLECYSTECTOMY TIMING FOR ACUTE CHOLECYSTITIS ON SHORT TERM SURGICAL MORBIDITY AND MORTALITY: A NSQIP DATABASE ANALYSIS
Fady Daniel*1, Maher Malaeb1, Mohammad N. Hosni1, Hani Tamim3, Aurelie Mailhac3, Mohammad khalife2, Walid N. Faraj2, Faek Jamali2
1Internal Medicine, Gastroenterology division, American University of Beirut Medical Center, Beirut, Lebanon; 2Surgery, American University of Beirut Medical Center, Beirut, Lebanon; 3Biostatistics Support Unit, Clinical Research Institute, American University of Beirut Medical Center, Beirut, Lebanon
Introduction:
Controversy exists about the best timing for cholecystectomy for acute cholecystitis (AC). There are mainly two approaches to dealing with AC: early surgery vs. initial conservative treatment followed by delayed cholecystectomy (several weeks later). However, there is growing evidence that supports early cholecystectomy is associated with better outcomes. Nonetheless, the exact timing of early cholecystectomy is still yet to be determined. The aim of this study is to elucidate the optimal timing of early cholecystectomy.
Methods:
We studied all patients undergoing open or laparoscopic cholecystectomy from the National Surgery Quality Improvement Program (NSQIP) participant use data specific file 2014-2016. NSQIP includes prospective validated outcomes and anonymized data for patients' demographics, functional statuses, preoperative risk factors, laboratory data, and 30-day postoperative outcomes for patients undergoing major surgery in more than 500 hospitals. The primary outcome in this study was short term surgical morbidity and mortality. The patients were divided into 4 groups, those who underwent surgery at days 0, 1, 2, 3+ for AC. We used the chi-square test to compare categorical variables between groups 0 and groups 1,2 and 3+ respectively. We used the independent t-test for continuous variables. We performed multivariate logistic regression to evaluate the association between the timing of surgery after admission and 30-days postoperative outcomes. We included confounders into the models based on both clinical and statistical significance.
Results:
A total of 21,392 patients were included. Laparoscopic approach was used in 86% of cases. The general characteristics of our population are presented in table 1. The overall morbidity (including wound infection, cardiac and respiratory complications, urinary infections, thromboembolism and sepsis) occurred in 1439 patients (6.82%), while 1-month rebleeding and mortality occurred in 457 (2.1%) and 185 (0.9%) patients, respectively (table 2). On univariate analysis, all morbidity events and mortality increased significantly with increased surgery timing from admission. Compared to patients who underwent surgery at day 0, and after adjusting for confounders (table 2), patients who underwent surgery at day 1 and day 2 had a significantly slightly lower composite morbidity. No significant difference among the four groups in the need for reoperation was noted. The bleeding rate was significantly higher in patients who were operated at day 2, and was highly significant in the 3+ group. Patients who underwent surgery at day 3+ had a significantly higher mortality rate.
CONCLUSION:
Early cholecystectomy performed after 72 hours from admission was associated with higher mortality and rebleeding. Our results support the "golden 72 hours window "for surgery in AC.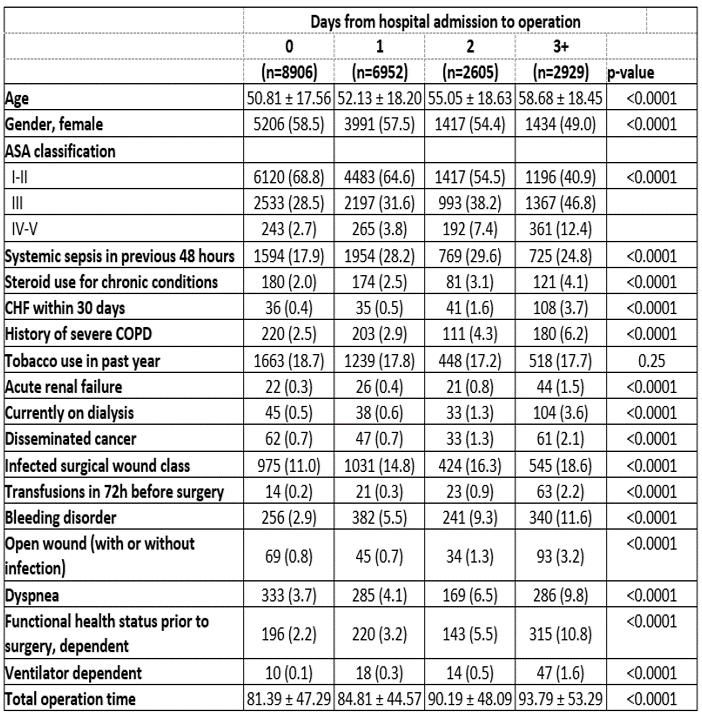
Table 1: Baseline demographic characteristics of the studied population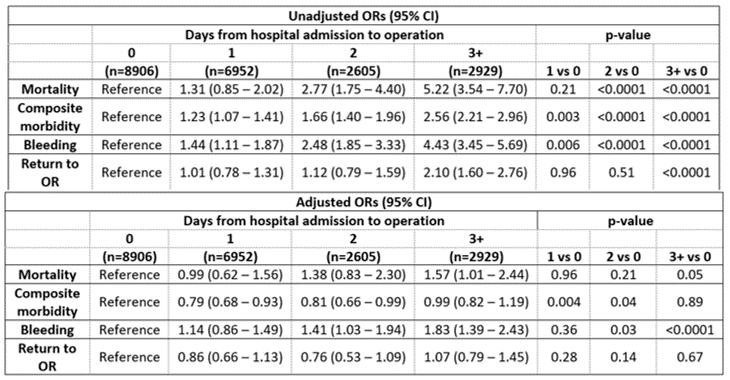
Table 2: Unadjusted and Adjusted outcomes
Back to 2019 Abstracts




