LYMPH NODE METASTASIS IN EARLY ESOPHAGEAL SQUAMOUS CELL CARCINOMA
Sophie L. Brigstocke*, Vaishali Patel, Saurabh Chawla, Parit Mekaroonkamol, Steven Keilin, Qiang Cai, Field F. Willingham
Digestive Diseases, Emory University School of Medicine, Atlanta, Georgia
Background: Esophagectomy with lymph node (LN) dissection is the treatment of choice for many patients with esophageal squamous cell carcinoma (ESCC). However, esophagectomy is associated with a high perioperative morbidity and mortality, and minimally invasive endoscopic management is now preferred for some patients with early-stage ESCC. The presence or absence of LN spread is a key determinant in establishing suitability for minimally invasive endoscopic management. Therefore, we analyzed a nationally representative dataset to determine the rates and predictors of LN involvement in patients with early-stage ESCC in a large, U.S. cohort.
Methods: The NCI's SEER database was queried for patients diagnosed with early-stage ESCC from 2004 -2015 with Tis, T1a or T1b disease who had undergone LN dissection for histologic confirmation. Patients with neo-adjuvant radiation were excluded. Data on LN positivity, tumor size, location, and grade were analyzed using SAS JMP.
Results: 558 cases of early stage ESCC met criteria for analysis. On univariate analysis, tumor stage, grade, and size were all significantly associated with LN metastasis for early squamous cell tumors (Table 1). T1b tumors had a LN metastasis rate of 29.7% versus 25.2% for T1a, and no LN spread for Tis tumors (p<0.001) (Figure 1). In terms of grade, 32.1% of high-grade tumors had LN spread versus 19.2% of low-grade tumors (p=0.011). Tumor size was also related to LN spread, with 13.3% of tumors < 2 cm having positive nodes compared to 33.2% of those > 2 cm (p=0.002). On multivariate analysis, tumor T-stage, tumor grade and tumor size were independently related to LN metastasis. Patients with high-grade tumors had a higher likelihood of LN spread compared to those with low-grade tumors (OR 1.91: 95% CI 1.16-3.15, [P =0.010]). Tumors > 2cm had a higher likelihood of LN metastasis compared with tumors < 2cm (OR 2.83: 95% CI 1.46-5.461, [P=0.002]). There was no significant association between LN spread and race, age or gender. The rate of LN spread was 4.35% for patients with low-grade, T1a tumors < 2cm in size. The rate of LN spread was 16.13% for patients with low-grade, T1b tumors <2 cm in size.
Conclusions: Tis ESCC and small, low-grade T1a tumors have low rates of LN involvement and represent a better population for endoscopic resection. For patients with T1b tumors, even small, low-grade tumors have relatively high rates of LN involvement, and as such, surgery with LN dissection may be indicated for patients who are considered good surgical candidates.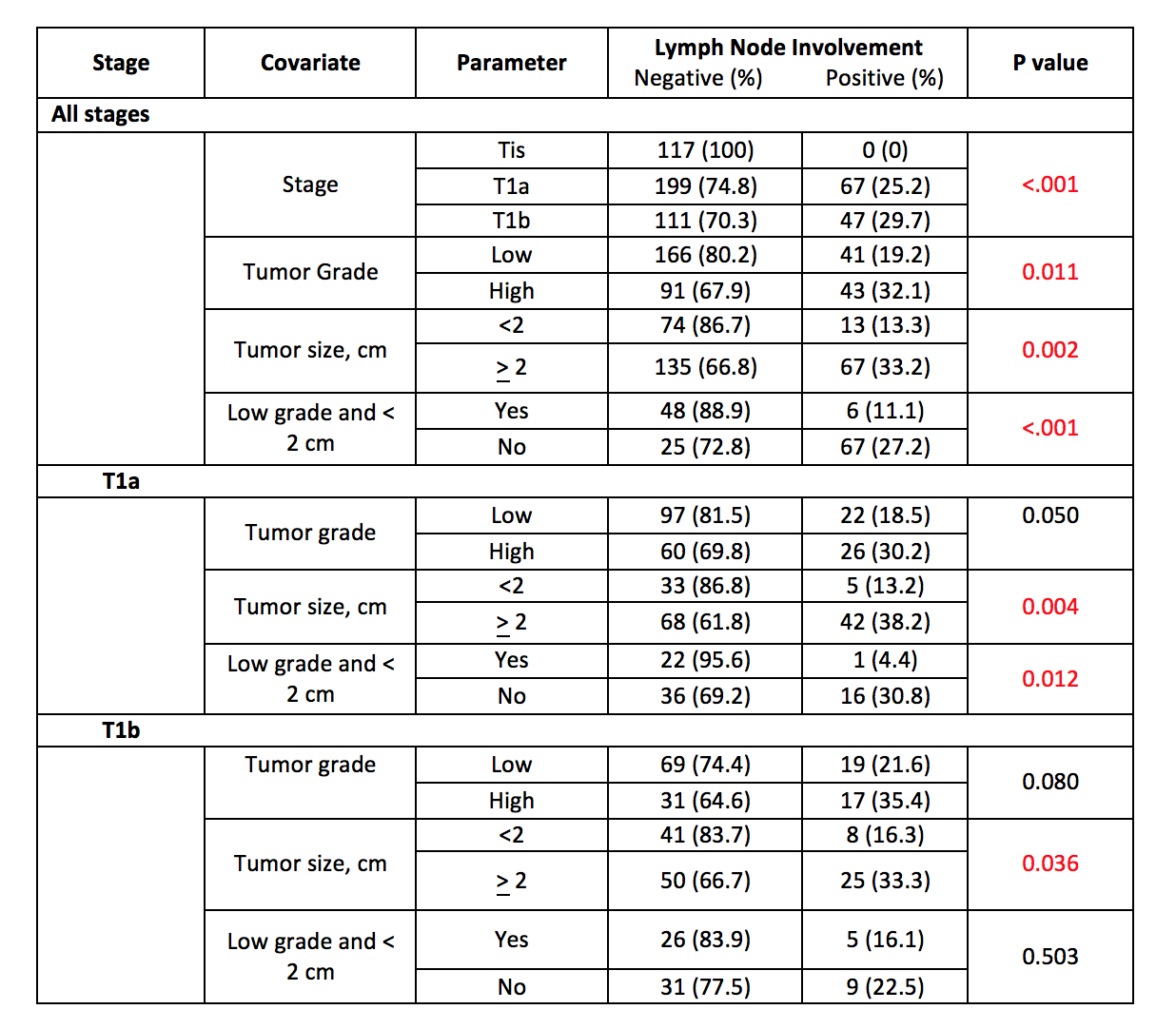
Table 1: Univariate Association Between LN Status and Covariates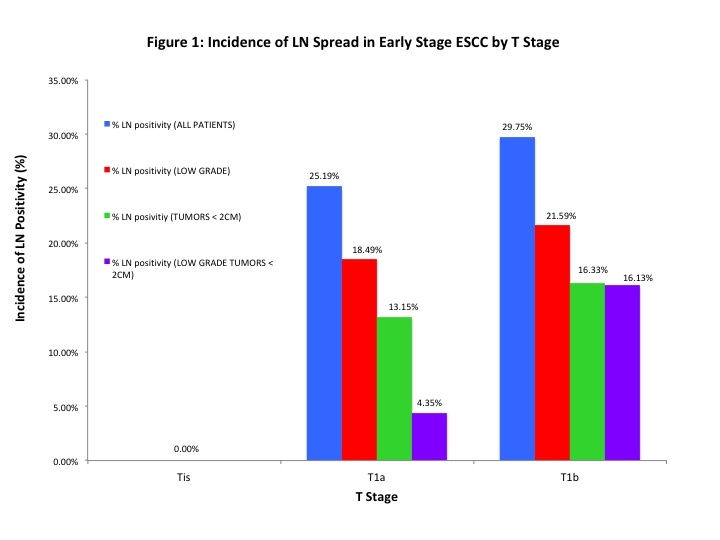
Back to 2019 Abstracts




