INSULIN CESSATION FOLLOWING LAPAROSCOPIC ROUX-EN-Y GASTRIC BYPASS VERSUS GASTRECTOMY
Keyvan Heshmati*, Jacqueline Hogan, Paul Sheils, Eric G. Sheu, Ali Tavakkoli
Surgery, Brigham and Women's Hospital, Boston, MA
Background: Bariatric surgery is widely considered the gold standard for weight loss and often leads to Type 2 Diabetes (T2D) remission. Insulin-treated (I-treated) patients are the most resistant group to complete T2D remission. However, coming off insulin treatment has a significant impact on the quality of life of patients. Therefore, we assessed rates and predictive factors of insulin cessation following Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG).
Methods: We performed a single institution, retrospective study of all I-treated T2D patients who underwent bariatric surgery between 2010-2015 (n=178). Data on demographics and T2D characteristics were recorded at baseline. Postoperative variables including Insulin use, weight, and HbA1c were collected up to 3 years of follow up. Statistical analysis was performed using a t-test, chi2, and longitudinal mixed-effects regression models.
Results: I-treated patients who underwent RYGB (n=102) and SG (76) presented with similar age (50 vs 52 years), sex (% female: 68 vs 57%), race (% white: 69 vs 67), BMI (43 vs 45 lb/in2), HbA1c (8.1 vs 7.9 %), and duration of T2D (12.4 vs 12.1 years), respectively (p>0.05). Following RYGB and SG, 37% and 47% of patients came off insulin at discharge, respectively (p=NS). Rates of insulin cessation remained relatively stable following SG during follow-up; however, insulin cessation continued to occur following RYGB (Figure 1A). From 1.5 years up to 3 years the proportion of patients who came off insulin was significantly greater following RYGB compared to SG (at 3-year: 62 vs 41%, respectively; p=0.04). RYGB led to greater weight loss than SG in the long-term in I-treated patients (3-year %TWBL: 26 vs 18%, respectively; p<0.001) (Figure 1B).
In a longitudinal mixed-effects regression model adjusted for demographics, %TBWL, and severity of T2D (Duration of diabetes, preoperative HbA1c, and number of insulin units per 24 hours), insulin cessation at discharge remained the most potent predictor of insulin cessation at any time up to 3 years following both RYGB (OR:11.2, 95% CI (3.7-33.7); p<0.0001) and SG (OR:62, 95% CI (8.8-441); p<0.0001).
Conclusions: RYGB and SG are effective and durable surgeries in assisting I-treated patients in stopping insulin use; however, RYGB leads to higher rates of insulin cessation longer term than SG. Insulin cessation occurs in a significant portion of patients as early as the time of discharge post-bariatric surgery. Insulin cessation at discharge is a strong and independent predictor of insulin cessation at any time up to 3 years postoperatively.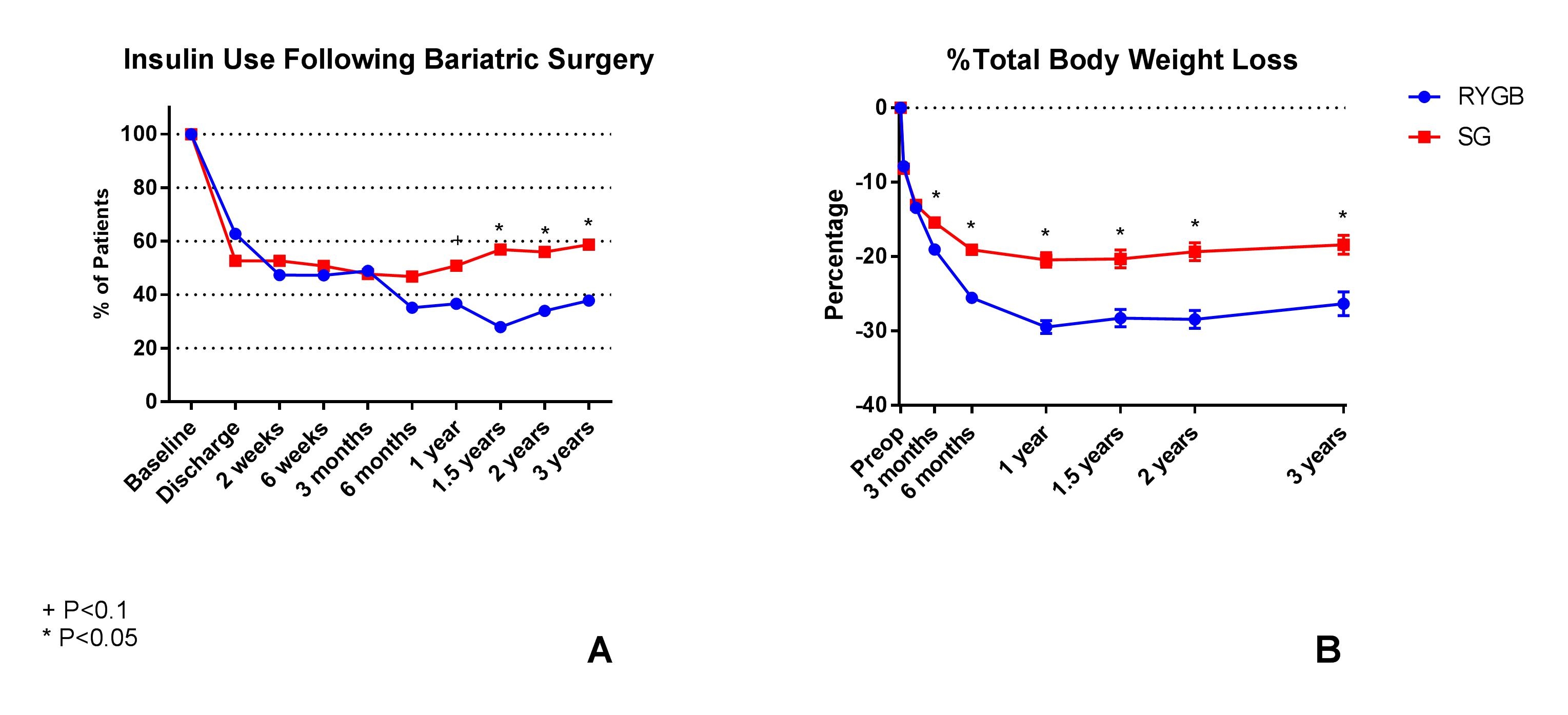
Figure 1. Percentage of patients who were on insulin following RYGB and SG (A). Percentage of total body weight loss following RYGB and SG (B).
Back to 2019 Abstracts




