SOCIOECONOMIC STATUS ALONE DOES NOT ENTIRELY EXPLAIN UNDERUSE OF HIGH-VOLUME CENTERS BY MINORITIES UNDERGOING ESOPHAGECTOMY
Tamar B. Nobel*1,2, Michael Curry1, David R. Jones1, Daniela Molena1
1Memorial Sloan Kettering Cancer Center, New York, NY; 2Mount Sinai Hospital, New York, NY
Background: Significant racial disparities have been demonstrated in the treatment of esophageal cancer. This is due, in part, to the observation that minority patients are less likely to be referred to a high-volume center (HVC) and have higher postoperative mortality. It is unclear why minorities are less likely receive care at HVC. The objective of this study was to evaluate the role of travel distance, insurance and socioeconomic status (SES) as factors associated with underuse of HVC by minorities undergoing esophagectomy.
Methods: Esophageal cancer patients that underwent esophagectomy for stage I-III between 2004-2015 were identified from the National Cancer Database. Median annual procedures per hospital was used to define volume: < 12 low volume center (LVC) and >12 HVC. "Nearby"? hospital was defined by median distance traveled. HVC use was compared by demographic and clinicopathologic characteristics. Chi square and Wilcoxon rank sum tests were used to compare categorical and continuous variables. To assess the impact of SES factors (insurance, education, income) on HVC use, we used two multivariable logistic regression models: 1 (baseline) included only tumor characteristics and demographics, and 2, which added SES factors to the model. The effect of HVC on 30-day and 90-day mortality was analyzed using multivariable logistic regression.
Results: A total of 21,898 patients underwent esophagectomy during the study period.
Black and Hispanic patients received surgery at HVC significantly less often than Whites (37% and 39% vs 50%; p<.0001). In model 1, Hispanic and Black patients had 37% and 39% lower odds of surgery at HVC as compared to Whites (p<.0001). (Table 1) After adjusting for SES factors in Model 2, the odds of HVC were still 35% lower for Blacks and Hispanics as compared to Whites (p<.0001).
The median distance traveled was 12.3 miles (IQR 5.5-29.9) to LVC as compared to 39.3 (IQR 15.5-88.4) for HVC (p<.0001). Black and Hispanic patients received care near their home more frequently than whites, regardless of hospital volume. (Figure 1)
After adjusting for clinicopathologic and socioeconomic factors, surgery at HVC independently decreased the odds of 30-day and 90-day mortality by 33% (OR 0.673. 95% CI 0.56-0.81) and 28% (OR 0.72, 95% CI 0.63-0.83), respectively.
Conclusions: Minorities are less likely to undergo esophagectomy at HVC despite improved short and long-term outcomes associated with increased surgical volume. Although insurance status and education are important determinants of HVC use, it seems that an important factor for minorities is to receive care near whether they live independent of hospital volume. Increased patient awareness and changes in physician referral patterns might increase use of HVC by minorities undergoing esophagectomy.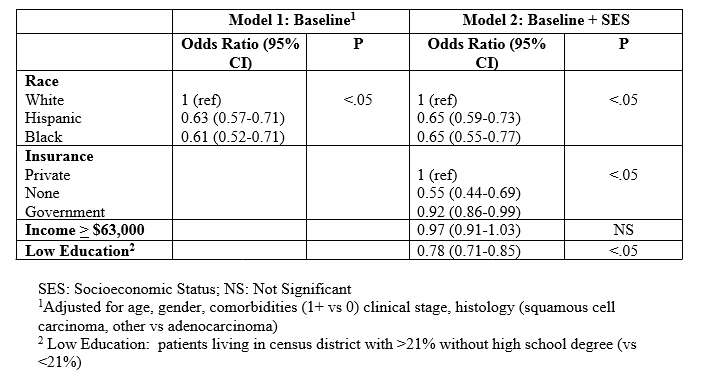
Table 1. Multivariate logistic analysis of factors predicting esophagectomy at a high-volume center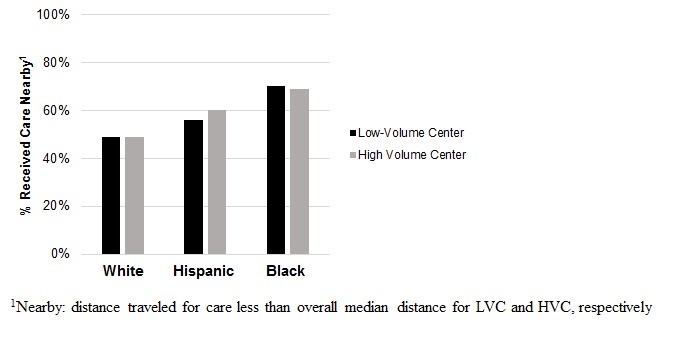
Figure 1. Percentage of patients that receive care near their homes by race and hospital volume
Back to 2019 Abstracts




