GASTROJEJUNAL ANASTOMOTIC STENOSIS: A TIME TO RE-INTERVENTION ANALYSIS COMPARING AXIOS STENT PLACEMENT TO GOLD-STANDARD BALLOON DILATION
Kelly Hathorn*1, Thomas J. Wang2, Pichamol Jirapinyo1, Jamila Wynter1, Ahmad Najdat Bazarbashi1, Thomas R. McCarty1, Marvin Ryou1, Christopher C. Thompson1
1Brigham & Women's Hospital, Boston, MA; 2Massachusett General Hospital, Boston, MA
Background: Gastrojejunal (GJ) anastomotic stenosis can be an unfortunate post-operative outcome, leading to severe, often difficult to manage symptoms of nausea, vomiting, and abdominal pain. Balloon dilation is considered the standard endoscopic treatment; however, recently placement of covered Lumen Apposing Metal Stents (LAMS) have shown promise. The aim of this study was to evaluate the efficacy of balloon dilation vs. LAMS placement for therapy of GJ stenosis.
Methods: This is a retrospective cohort study performed at two major academic institutions. The Research Patient Data Registry (RPDR) was used to extract all patients who had documentation of a GJ stenosis. Among these patients, eligible patients were adults (age >/= 18) with a benign etiology of stenosis whom underwent endoscopic treatment. Baseline patient characteristics (age, sex, date of surgical revision if applicable) were obtained. Procedure specific data, including use of balloon dilation, fluoroscopy-guided dilation, steroid or mitomycin injection, incisional therapy, and/or AXIOS stent placement, were assessed. Primary outcome was time-to-reintervention or surgical revision. Secondary outcome was procedure-related complication. Fischer's exact, student T-test, Kaplan-Meier analyses were performed.
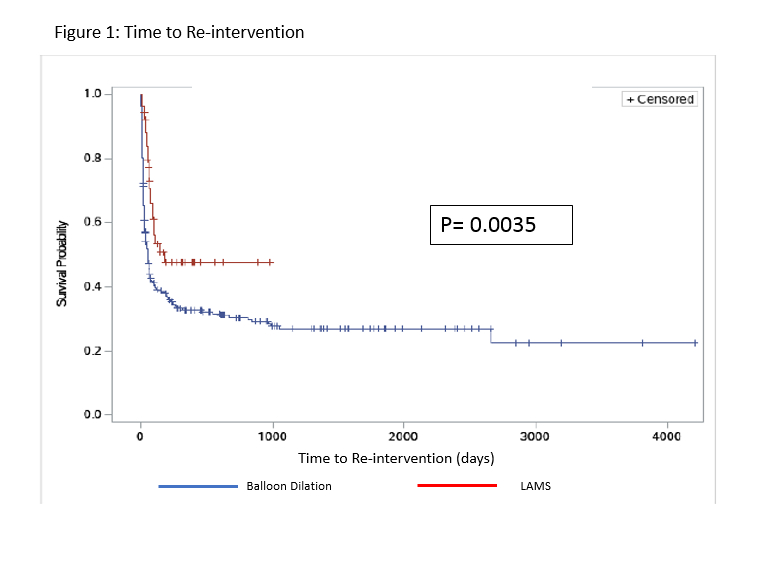
Results: Overall, there were 118 patients with GJ stenosis. Baseline characteristics are summarized in Table 1. There were 319 endoscopic interventions performed (274 balloon dilations, 53 LAMS placements), with mean number of interventions per patient of 3.09 ± 2.29. Average GJ size at onset of procedure was 7.48 ± 3.8 mm, and ulceration was noted in 24% of cases. The median time to re-intervention or surgical revision after balloon dilation was 49 days, whereas the median time after LAMS placement was 175 days (p=0.0035, Figure). 22% (26/118) of patients ultimately required surgical revision. There were procedure-related complications in only 3 of the 319 procedure (0.94%); all three cases were related to balloon dilation and included one jejunal tear (no frank perforation but required stent placement), one mucosal tear with bleeding requiring stent placement, and one mucosal tear with bleeding requiring hemostatic clip placement. Expected mucosal tears from balloon dilation were not included in this analysis.
Conclusion: Balloon dilation and LAMS placement are both safe treatment options for GJ stenosis. While LAMS placement is typically reserved for refractory cases, on time-to-event analysis, LAMS placement had a longer time to re-intervention. Thus, although more data is required from a cost utility perspective, these data suggest that it may be beneficial to consider LAMS placement earlier in the treatment course for benign GJ stenosis.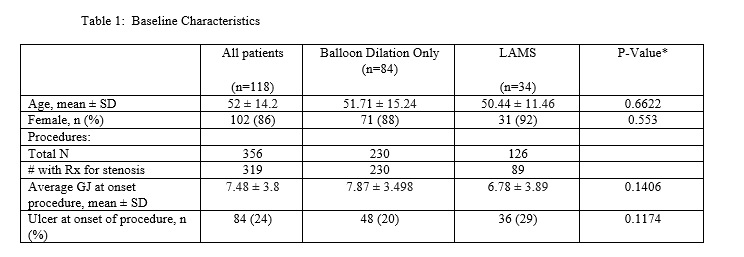
Back to 2019 Abstracts




