OUTCOME PREDICTOR SCORE FOR MULTIVISCERAL RESECTION IN T4 GASTRIC CANCER
André R. Dias2, Marina A. Pereira2, Marcus F. Ramos2, Bruno Zilberstein1, Ivan Cecconello1, Ulysses Ribeiro*2,1
1Gastroenterology, University of São Paulo, Sao Paulo, SP, Brazil; 2Gastroenterology, Sao Paulo State Casncer Institute - University of Sao Paulo School of Medicine, ICESP-HCFMUSP, Sao Paulo, Brazil
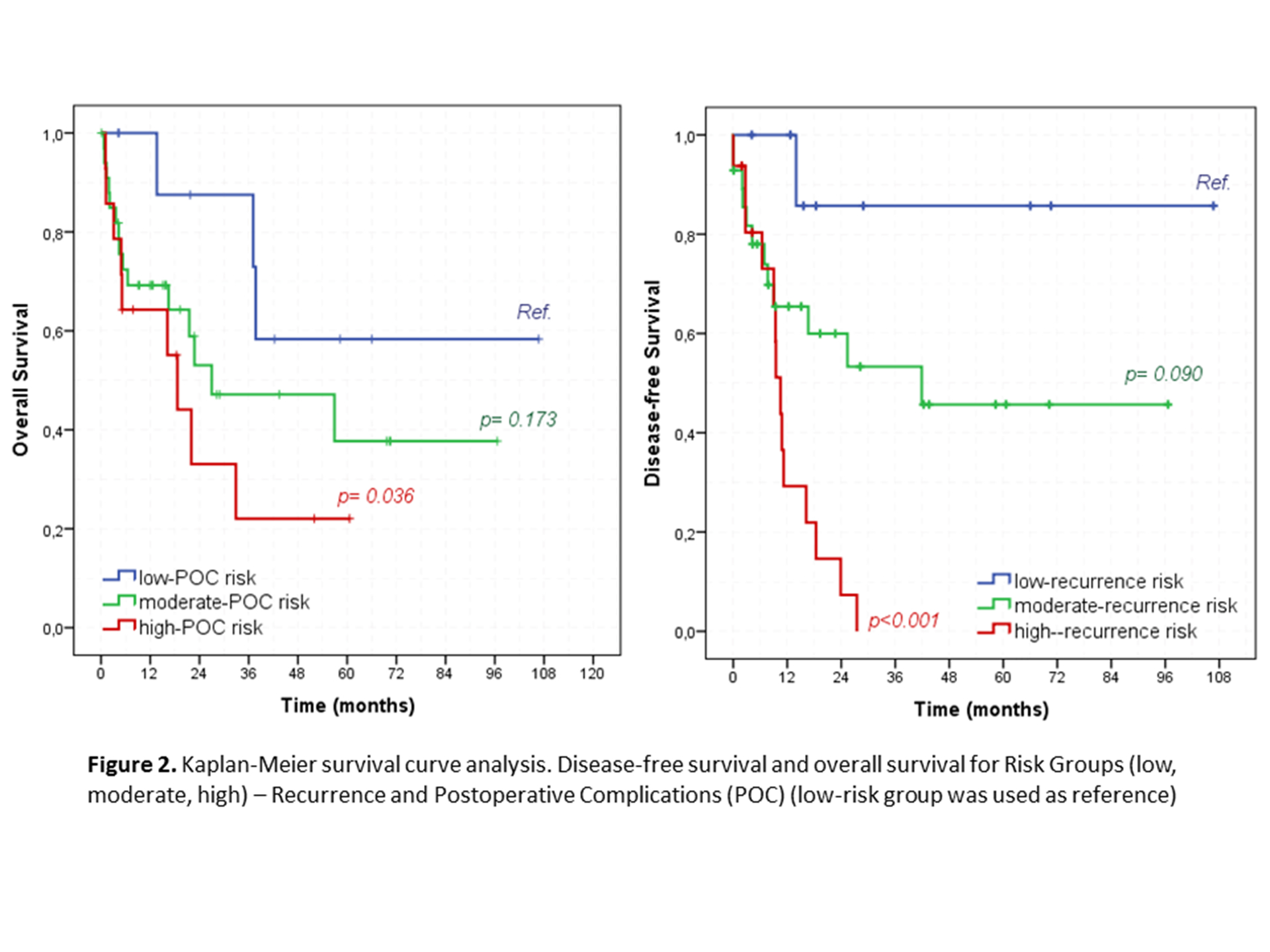
Introduction: Multivisceral resection (MVR) is indicated in T4b gastric cancer when R0 can be achieved. Patient`s selection for MVR is imperative, since it carries an increased risk for postoperative complications (POC). Additionally, some patients may have an early recurrence not benefiting from the procedure. Currently, we lack data concerning patient`s selection and an objective score system is desired. Objective: to develop a scoring system to predict POC and disease recurrence in gastric adenocarcinoma patients eligible for MVR. Methods: From a prospective database, we selected those who underwent MVR due to adjacent organ invasion (cT4b). Inclusion criteria were: gastric adenocarcinoma, cT4b lesions, curative intent surgery. Scoring models for postoperative complications (POC) and recurrence were created based on the variables identified by binary regression, and cutoff values established using ROC curve. A prognostic index was constructed, dividing the patients in 3 risk groups: low (<15%), intermediate (15-75%) and high (>75%). Results: In 1043 patients, 237 had MVR, of these 58 fulfilled all inclusion criteria. Most were men (70.7%), and the mean age was 61.8 years. Twenty-nine patients had 1 additional organ resected and the remaining 29 had 2 or more. The most resected organ was the pancreas (76%), followed by spleen (56%), colon (50%) and liver (24%). The mean lymph node yield was 44, pT4b was confirmed in 34 cases (58,6%) and 74.1% of the patients had lymph node metastasis. Major POC occurred in 25.9% of cases, with surgical mortality of 8.6%. The median Overall survival (OS) and Disease free survival (DFS) were 32.9 and 18.4 months, respectively. No differences were observed in OS and DFS between pT4b and non-pT4b GC cases (p=0.241 and p=0.258, respectively). DFS was significantly worse for pN+ than pN0 (41.5% vs 75%, p=0.044) and for patients with 3-4 additional organs resected compared to 1-2 structures (27.3% vs 54.8, p=0.026). For the score model, five parameters were identified as positive predictive factors for POC and 6 for recurrence. The POC-score had accuracy of 80.6% (95%CI=0.69-0.92) and recurrence-score of 78% (95%CI=0.66-0.90), with cut-off value of 50.5 and 62.9, respectively (Figure 1). OS was better in the low-POC group compared to high-and intermediate-POC. DFS was also better according to the recurrence risk: low: 88.9%; moderate: 57.1%; high:12.5% (p<0.001) (Figure 2). Conclusion: The scoring system based on clinicopathologic parameters accurately predict POC and recurrence in patients with gastric adenocarcinoma undergoing MVR. Classification of these patients allows for an individualized approach.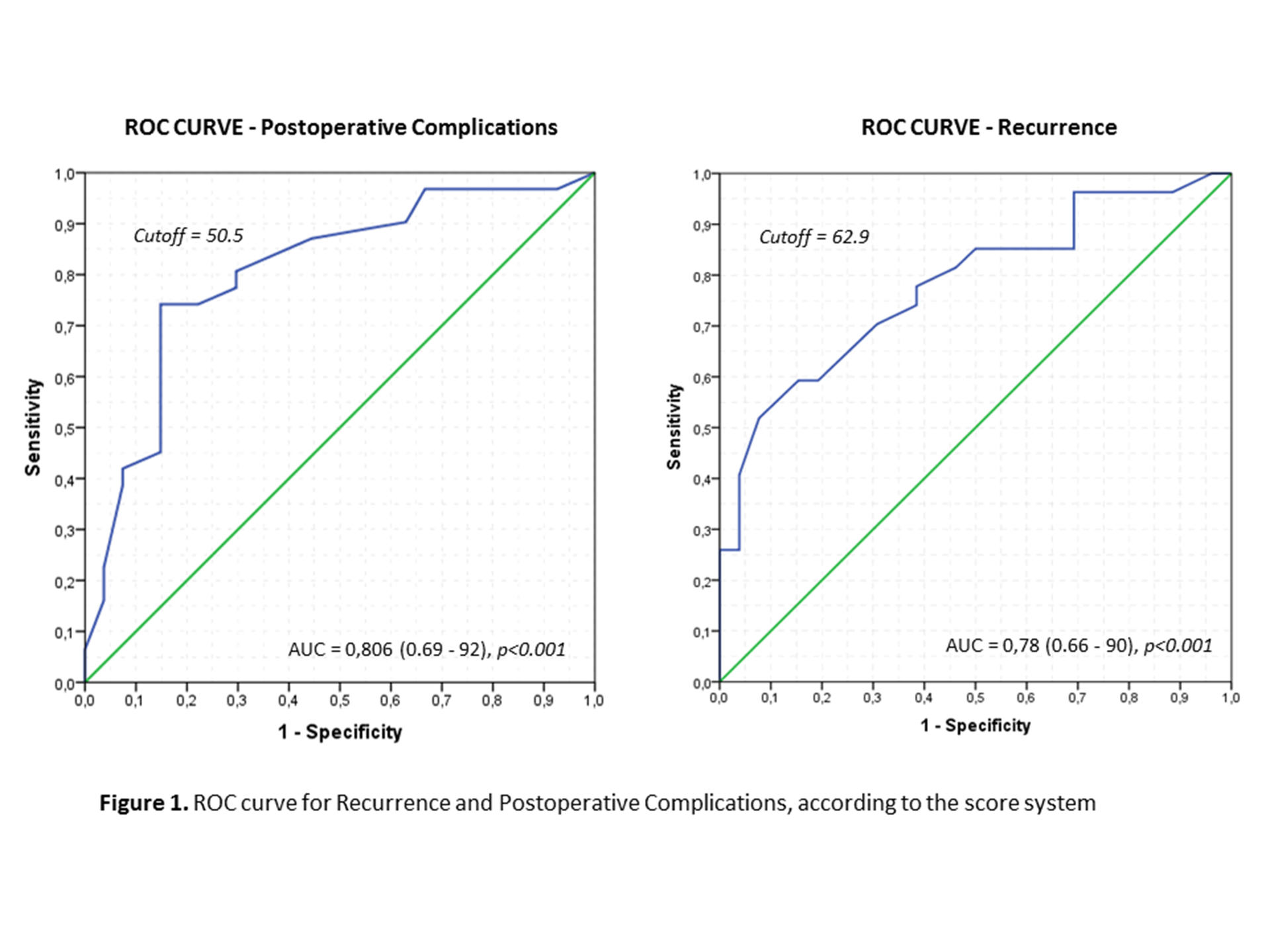
Back to 2019 Abstracts




