HIGH RESOLUTION MANOMETRY CHANGES IN PATIENTS WITH ACHALASIA AFTER LAPAROSCOPIC HELLER MYOTOMY WITH PARTIAL FUNDOPLICATION
Emmanuel Contreras Jiménez*2, Enrique Coss-Adame1, Miguel A. Valdovinos1, Janette Furuzawa-Carballeda1, Sofia Narvaez-Chavez1, Hector Olvera-Prado1, Jose Peralta-Figueroa1, Gonzalo Torres-Villalobos2
1National Institute of Medical Sciences and Nutrition Salvador Zubiran, Mexico City, Mexico; 2Surgery Division, National Institute of Medical Sciences and Nutrition Salvador Zubiran, Mexico City, Mexico
Introduction:Achalasia is classified by high-resolution manometry (HRM) into three subtypes, and this classificationcorrelates with the outcome. Laparoscopic Heller myotomy (LHM) with partial fundoplication is an effective treatment for achalasia. Currently there are just few studies that describe postoperative evaluation by HRM and its possible correlation with results after surgery.
Objective: To analyze manometric changes in patients with primary achalasia after LHM with partial fundoplication (Dor vs.Toupet).
Methodology:This was a randomized (Dor or Toupet) and prospective controlled trial after LHM. HRM, upper endoscopy and barium esophagogram were performed preoperatively in all patients. The postoperative evaluation was performed at 1, 6, 24 and 48 months. Symptoms analysis were performed with the Eckardt and EAT-10 questionnaires.
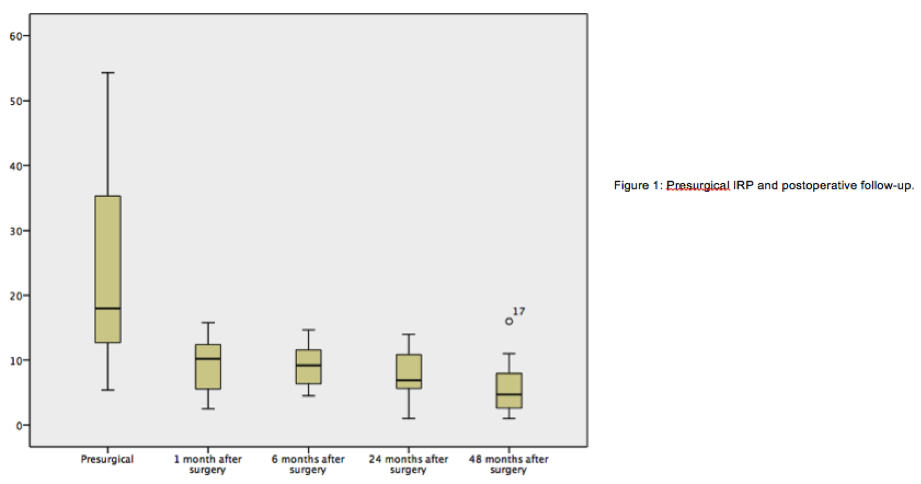
Results:Ninety-four patients with primary achalasia were included. 51.1% patients underwent Dor and 48.9% Toupet. Baseline characteristics were similar between groups. The median age was 40 years and 60.6% were women. Lower esophageal sphincter pressure and integrated relaxation pressure (IRP) showed a significant decrease at one month after surgery (p <0.001) with persistence of the changes throughout the follow-up (figure 1). The type of fundoplication performed did not show any manometric differences between the two groups. According to the symptom scores, there was clinical improvement in all the follow-up (p <0.001). There was not significant correlation between clinical improvement and changes in the manometric pattern.
Conclusions:There were important manometric changes after performing a LHM in patients with achalasia, mainly a decrease of the IRP and the lower esophageal sphincter pressure during the four years follow-up. These changes are not associated with the type of partial fundoplication (Toupet and Dor). Clinical improvement was evident after LHM with fundoplication.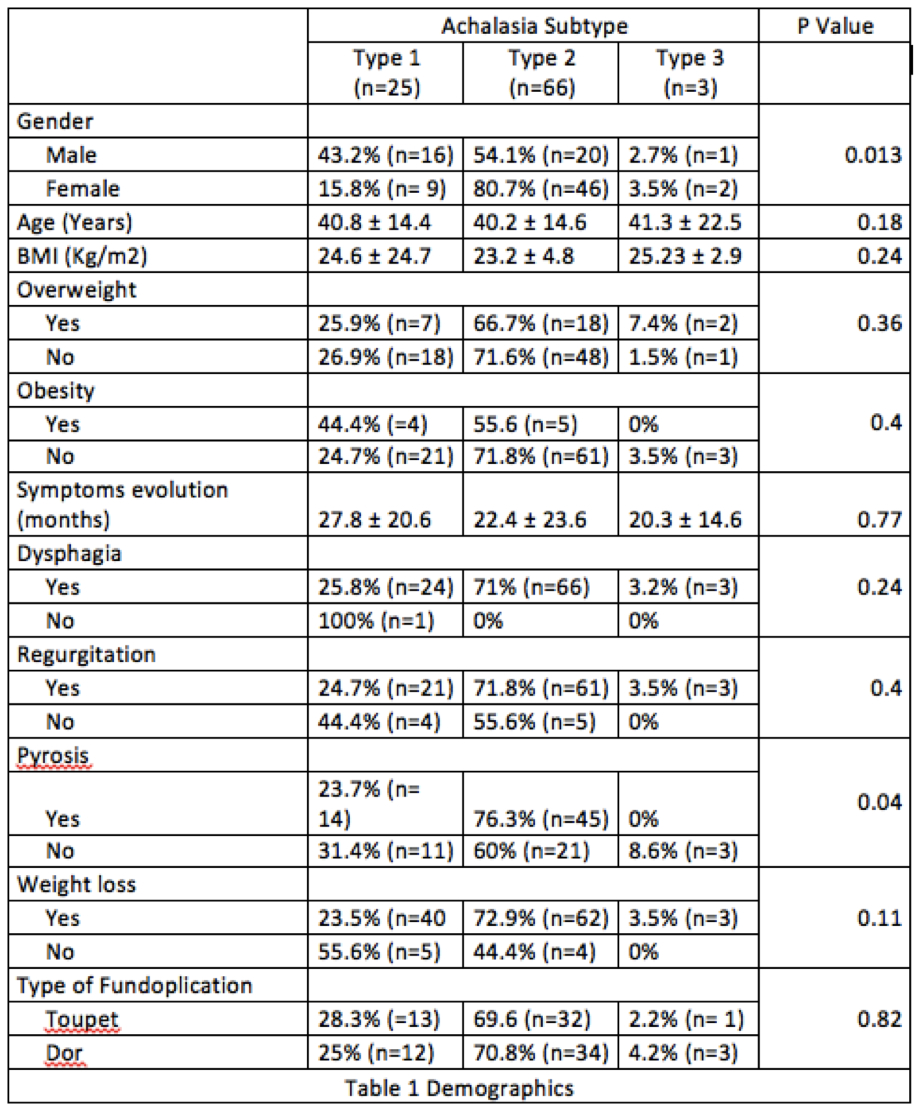
Back to 2019 Abstracts




