ACCELERATION OF POSTOPERATIVE RECOVERY WITH BRIEF INTRAOPERATIVE VAGAL NERVE STIMULATION MEDIATED VIA THE AUTONOMIC MECHANISM
Alimujiang Maisiyiti*1,2, Yan Meng1,3, Xue Lin1,4, Yiling Zhang1,5, Payam Gharibani1, Jiande Chen1
1Johns Hopkins University, Baltimore, MD; 2Department of Minimally Invasive Surgery, hernias and abdominal wall surgery, People's Hospital of Xinjiang Uyghur Autonomous Region, Urumqi, China; 3Department of Gastroenterology, Nanfang Hospital, Southern Medical University, Guangzhou, China; 4Department of Gastroenterology, College of Integrative Medicine, The First Affiliated Hospital of Dalian Medical University, Dalian, China; 5School of Life Science, Beijing University of Chinese Medicine, Beijing, China
Background/Aims:Postoperative recovery is the main influencing factor in hospital stay and patients' satisfaction. The aim of this study was to investigate the effects and mechanisms of the intraoperative vagus nerve stimulation (iVNS) on postoperative recovery from abdominal surgery in rats.Methods: Rats were randomly divided into sham-iVNS group (n=9) and iVNS group (n=9). The Nissen fundoplication surgery was performed in both sham-iVNS (no stimulation during surgery) group and iVNS (30-min VNS during surgery via electrodes at sub diaphragm) group. In addition to Nissen fundoplication, iVNS was performed in iVNS group. Animal's behavior, eating, drinking and feces' conditions were monitored at specific postoperative periods. Gastric slow waves (GSWs) and electrocardiogram (ECG) were recorded. Blood samples were collected for inflammatory cytokines levels in plasma.Results: 1) iVNS accelerated postoperative recovery by shortening initiate time to drink(28.4±3.9 min vs 58.3±15.9 min,p<0.001, vs. sham-iVNS) and eat (37.6±3.5 min. vs 66.0±20.1 min,p<0.01, vs. sham-iVNS), increasing the number of fecal pellets (POD1: 28.0±5.03 vs15.2±5.31, p<0.01, vs. sham-iVNS) and percentage of water content in fecal pellets(52.8% vs. 35.9%, P<0.01, vs. sham-iVNS). 2) iVNS improved gastric pace-making activity at 6 hrs after surgery: a higher percentage of normal slow waves was observed in the iVNS group compared to the sham-iVNS group(67.9±12.7% vs 52.2 ±11.8%, p<0.05, vs. sham-iVNS). 3) iVNS improved vagal activityat 6 hrs (0.58±0.12 vs 0.38±0.09, p<0.01, vs. sham-iVNS) and 24hrs (0.57±0.08 vs 0.49±0.05, p<0.05) after the surgery. Increased vagal tone was correlated with a faster postoperative recovery to start water (r=-0.623, p<0.01) and food (r=-0.594, p<0.01) intake.4) The concentrations of TNF-α, IL-1β and IL-6in plasma were increased after surgery in both sham-iVNS and iVNS group, and this increase was reduced in iVNS group compared to sham-iVNS group. (TNF-α: 311.9±48.9 vs 392.9±34.7, p<0.01; IL-1β: 167.2±28.4 vs 196.5±26.3, p<0.05; IL-6: 152.9±18.2 vs 182.5±16.4, p<0.01). Conclusions: Brief intra-operative VNS accelerates postoperative recovery by enhancinggastric pace-making mediated via the autonomic-cytokine mechanisms.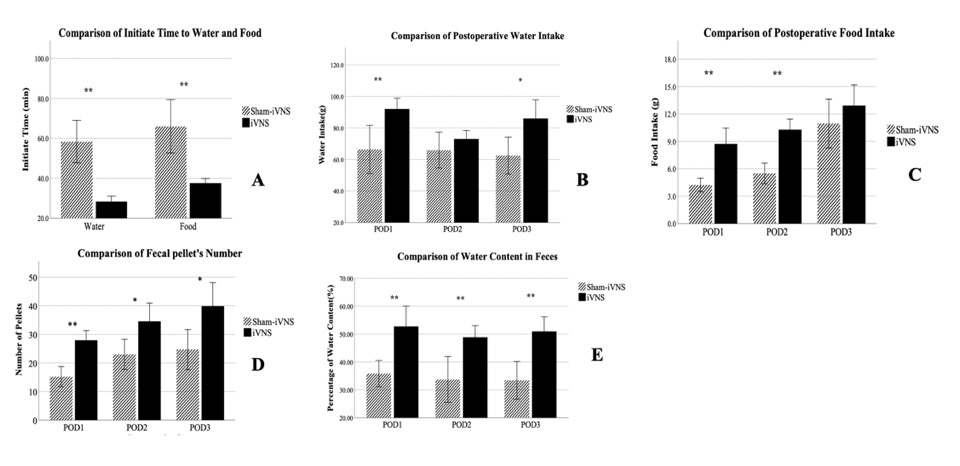
Fig.1 Effects of iVNS on Postoperative Animal Behaviors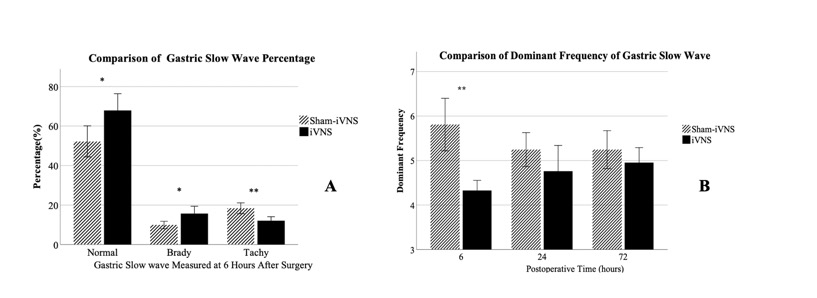
Fig.2 Mechanisms of iVNS Involving Gastrointestinal Motility
Back to 2019 Abstracts




