OUTCOMES AND PREDICTORS OF OF MORBIDITY FOLLOWING SURGICAL DRAINAGE OF PANCREATIC PSEUDOCYSTS
Sean Neifert*, Jeanie Gribben, Nicole Ilonzo, I. Michael Leitman
Surgery, Icahn School of Medicine at Mount Sinai, New York, NY
Introduction:
Pancreatic pseudocysts have been reported to occur in up to 15% of cases of pancreatitis, making them the second most common indication for pancreatic surgery behind malignancy. Endoscopic internal drainage has become favored recently; however, there are still a cohort of patients who undergo external or internal surgical drainage. The objective of the present study is to compare outcomes of common surgical drainage procedures.
Methods:
Patients undergoing a pancreatic pseudocyst drainage via open drainage (OD), loop cystojejunostomy (LCJ), and Roux-en-Y cystojejunostomy (RYCJ) were queried from the American College of Surgeons National Surgical Quality Improvement Program from 2014-2017. Data were analyzed based upon demographics, comorbidities, and complications following drainage. Statistical analysis was performed using chi-square, Student's t-test, and multivariable logistic regression.
Results:
A total of 102 patients underwent LCJ, 75 underwent OD, and 161 underwent RYCJ. There were no differences in the mean age or gender distribution of the cohorts. Those undergoing OD had higher ASA classes when compared to the LCJ (p=0.05) and RYCJ (p=0.01). The OD cohort had higher rates of preoperative sepsis than both the LCJ (33.33% vs. 13.73%, p=0.002) and the RYCJ cohorts (33.33% vs. 11.80%, p<0.0001). Those patients in the RYCJ cohort also had lower rates of hypertension (44.10% vs. 60.00%, p=0.02) and COPD (10.67% vs. 1.86%, p=0.005) than the OD cohort. Those undergoing LCJ (70.59% vs. 36.00%, p<0.0001) and RYCJ (53.42% vs. 36.00%, p=0.01) were also significantly more likely to be undergoing the procedure electively.
In the cohorts undergoing LCJ (0.62% vs. 6.67%, p=0.01) and RYCJ (0.00% vs. 6.67%, p=0.01), there were significantly fewer deaths than those in the OD cohort. Furthermore, the LCJ cohort (13.66% vs. 24.00%, p=0.049) was less likely to suffer a wound complication than the OD cohort, but this finding did not endure in multivariable modeling (Odds ratio [OR]: 1.17; 95% Confidence Interval [CI]: 0.57 - 2.43; p=0.67). The LCJ patients were less likely to suffer a complication than the OD patients (OR: 0.49; 95% CI: 0.26 - 0.89; p=0.02), and the RYCJ comparison, while also initially significant (35.29% vs. 57.33%, p=0.004), lost significance during adjusted modeling (OR: 0.54; 95% CI: 0.28 - 1.05; p=0.07).
Conclusions:
Patients undergoing OD have more comorbid illness than those undergoing LCJ and RYCJ. Patients undergoing LCJ still had lower rates of complications than patients undergoing OD after multivariable modeling to account for these factors.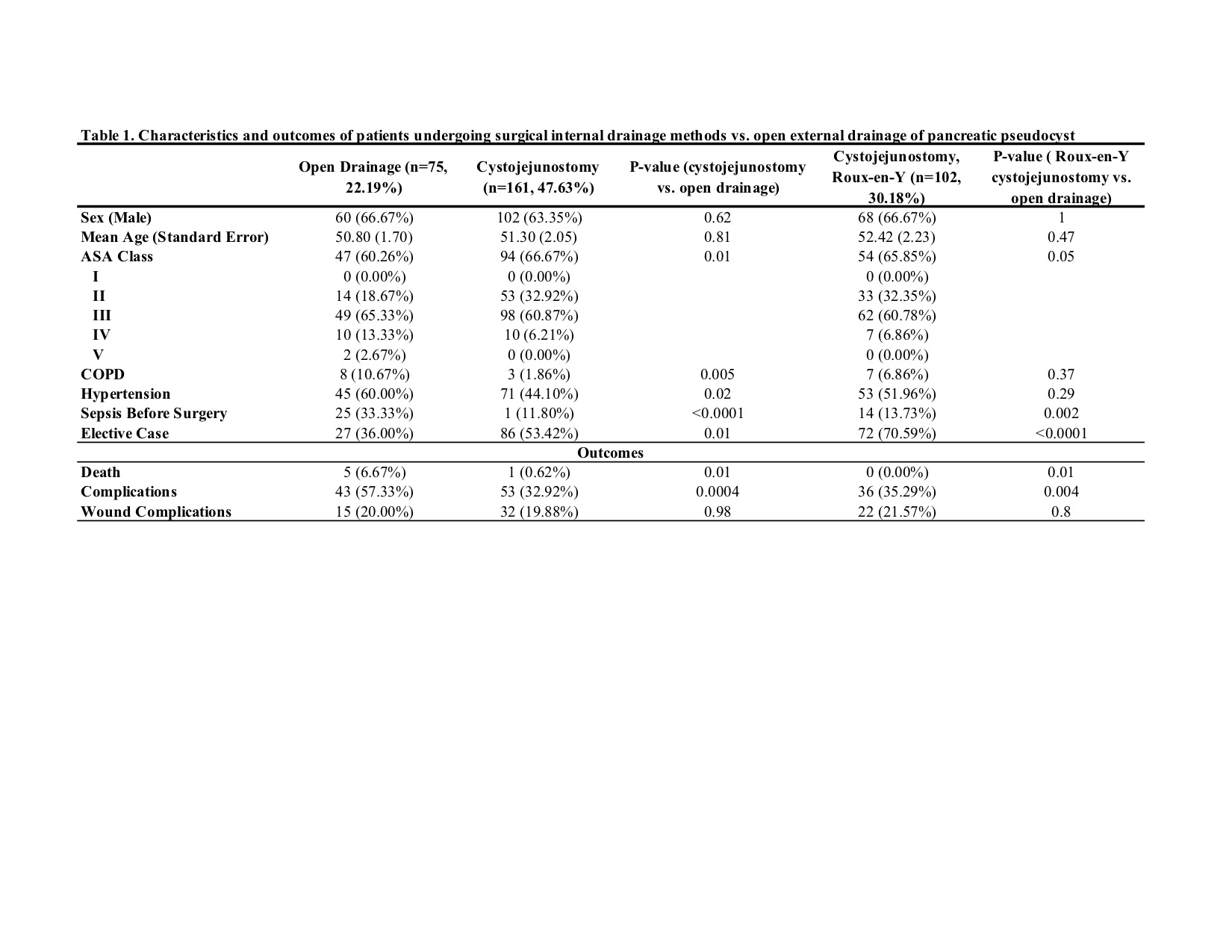
Back to 2019 Abstracts




