NEOADJUVANT CHEMOTHERAPY FOR PANCREATIC DUCTAL ADENOCARCINOMA IMPROVES SURVIVAL AND R0-RATE EVEN IN STAGE I
Onur C. Kutlu*1, Eduardo A. Vega4, Sandeep Krishnan5, Jeffrey Wisch3, Frank Pomposelli2, Dicken Ko2, Danny Sleeman1, Nestor de La Cruz1, Claudius Conrad2
1Surgery, University of Miami, Miami, FL; 2Surgery, St Elizabeth's Medical Center, Boston, MA; 3Dana-Farber Cancer Institute, Boston, MA; 4Surgical Oncology, UT MD Anderson Cancer Center, Boston, MA; 5Internal Medicine, St Elizabeth's Medical Center, Boston, MA
Background: Preoperative chemotherapy in pancreatic adenocarcinoma (PDAC) provides early treatment of micrometastatic disease, reduces positive surgical margin rates, identifies patients with rapidly progressive disease and assures that surgical candidates will receive chemotherapy even in case of postoperative complications. However, limited data is available on the impact of neoadjuvant chemotherapy on very early PDAC (Stage IA).
Material and Methods: Pancreaticoduodenectomy patients for PDAC between 2010 and 2014 were identified in the National Cancer Data Base (NCDB). Early-stage patients (IA-IB) with complete oncologic and clinical information and more than 30-day survival were included. The effect of neoadjuvant therapy on margin status was assessed with binary logistic regression. The effect of therapy sequencing and comparison of preoperative (NCT), postoperative (ACT), perioperative (pre and post-OP, PCT) chemotherapy and surgery only (SURG) was analyzed using Cox regression, correcting for age, sex, grade, margin status, hospital volume and hospital setting (community, academic center, NCI designated cancer center).
Results: Of 4,231 patients, 602 (14.2%) were Stage IA, and 3629 (85.8%) IB. The rate of NCT was only 8.1%. Rate of margin positivity was 19.1% for the entire cohort and lower for NCT (12.3 vs 19.7%). After correcting for confounders, the risk of a positive margin was lower in NCT (OR 0.703, 95% CI 0.500-0.988, p=0.042). Cox regression showed a significant overall survival advantage for NCT (p=0.003, HR 0.799), ACT (p=0.001, HR 0.749) and PCT (p<0.001, HR 0.706) compared to SURG. There was no difference in survival between chemotherapy groups with a trend towards optimal survival for PCT.
Conclusion: Neoadjuvant Chemotherapy results in lower risk of a positive surgical margin and improved survival compared to surgery alone even in stage IA PDAC. These results suggest that PCT should be strongly considered in all patients with resectable PDAC, including very early PDAC cases.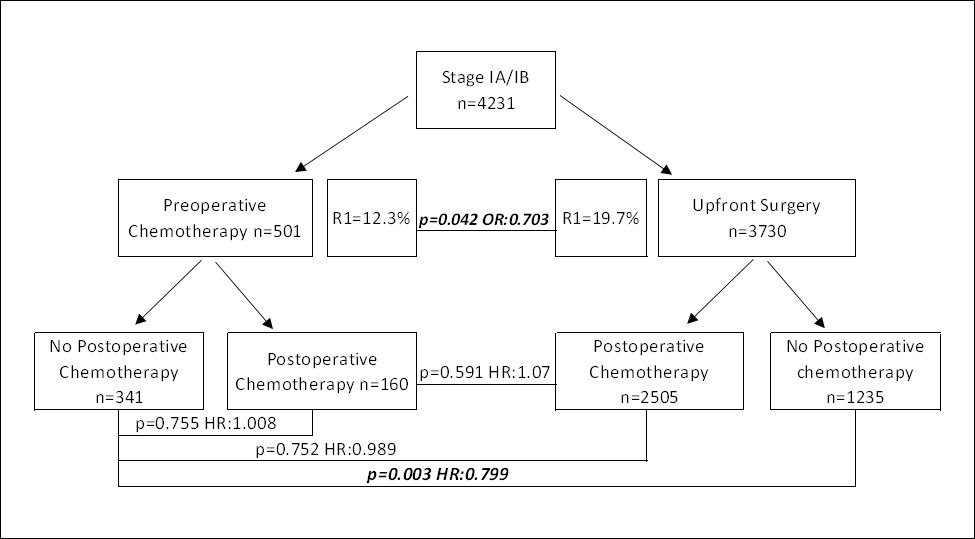
Back to 2019 Abstracts




