THE IMPACT OF PANCREATIC DUCTAL DISRUPTION ON THE OUTCOME OF ACUTE PANCREATITIS: RESULTS FROM A PROSPECTIVE STUDY
SRIRAM R. DEIVASIGAMANI*1, Rajesh Gupta2, Surinder S. Rana3, Mandeep Kang4, Harjeet Singh2, Vishal Sharma3
1GENERAL SURGERY, POST GRADUATE INSTITUTE OF MEDICAL COLLEGE AND RESEARCH INSTITUTE, Chandigarh, Chandigarh, India; 2DIVISION OF SURGICAL GASTROENTEROLOGY, POST GRADUATE INSTITUTE OF MEDICAL COLLEGE AND RESEARCH INSTITUTE, CHANDIGARH, CHANDIGARH, India; 3MEDICAL GASTROENTEROLOGY, POST GRADUATE INSTITUTE OF MEDICAL COLLEGE AND RESEARCH INSTITUTE, CHANDIGARH, CHANDIGARH, India; 4RADIO DIAGNOSIS, POST GRADUATE INSTITUTE OF MEDICAL COLLEGE AND RESEARCH INSTITUTE, CHANDIGARH, CHANDIGARH, India
Background:
Pancreatic duct disruption (PDD) is a recognized complication of acute necrotising pancreatitis (ANP). Early recognition of PDD in the course of ANP could permit appropriate intervention before complications develop. Studies exploring impact of PDD in ANP are lacking. We aimed to study the incidence, clinical characteristics and outcome of patients with PDD in ANP.
Methods:
Prospective single centre observational study conducted from January 2017 to June 2018. Patients with severe and moderately severe ANP (revised Atlanta classification) were included. Patients on life support, mild pancreatitis, and those in whom MRCP was contraindicated, were excluded. MRCP was done 7 days after onset of symptoms. PDD was diagnosed by- pancreatic necrotic segment of 2 cm, viable upstream pancreatic tissue from the site of necrosis or communication between main pancreatic duct (MPD) and peripancreatic collection. Statistical analysis was performed between data points of interest.
Results:
A total of 32 patients were studied. The incidence of PDD was 40.6% (n=13). Mean age of the study population with PDD was 33.5+12.9 years, with M:F ratio of 2.5:1. Most frequent etiology associated with PDD was alcohol (46.2%) followed by gallstones (23.1%). Most common region of disruption was pancreatic neck in 53.8%.
Patient with PDD were more likely to develop multiple organ failure (p=0.029), and had significantly higher median APACHE II scores at presentation (p=0.03) and at the time of MRCP (p<0.001) and median MMS at presentation (p=0.03) and at the time of MRCP (p<0.001). Patients with PDD also had higher median CTSI score (p=0.001), higher MRSI score (p=0.002) and increased chances of developing splenic vein thrombosis (p<0.001), ascites (p=0.001) and pleural effusion (p=0.001). Presence of PDD significantly prolonged the total hospital stay (p=0.002) and ICU stay (p=0.002).
PDD was successfully managed by ERCP stenting (46.1%) without requirement of surgery. Surgical necrosectomy was needed in 3 patients, for uncontrolled sepsis with persistent organ failure, and all 3 patients had PDD. There were 2 mortalities in the study cohort, both occurring in patients with PDD.
APACHE II value > 9.0 had sensitivity of 92.3% and specificity of 96% and MMS value > 3.0 had sensitivity of 84.6% and specificity of 78.9% in predicting PDD at presentation. Drain fluid amylase value > 6943 U/L had sensitivity of 100% and specificity of 94.7% for presence of PDD.
Conclusion:
In patients with ANP, presence of PDD significantly increases morbidity. Nearly half of PDD required ERCP and stenting for successful management. Early MRCP in first week of illness can be used to diagnose PDD with high accuracy rate. Variables like APACHE II score and MMS score at presentation and drain fluid amylase value in patients with PCD can be used as a marker to predict the presence of PDD.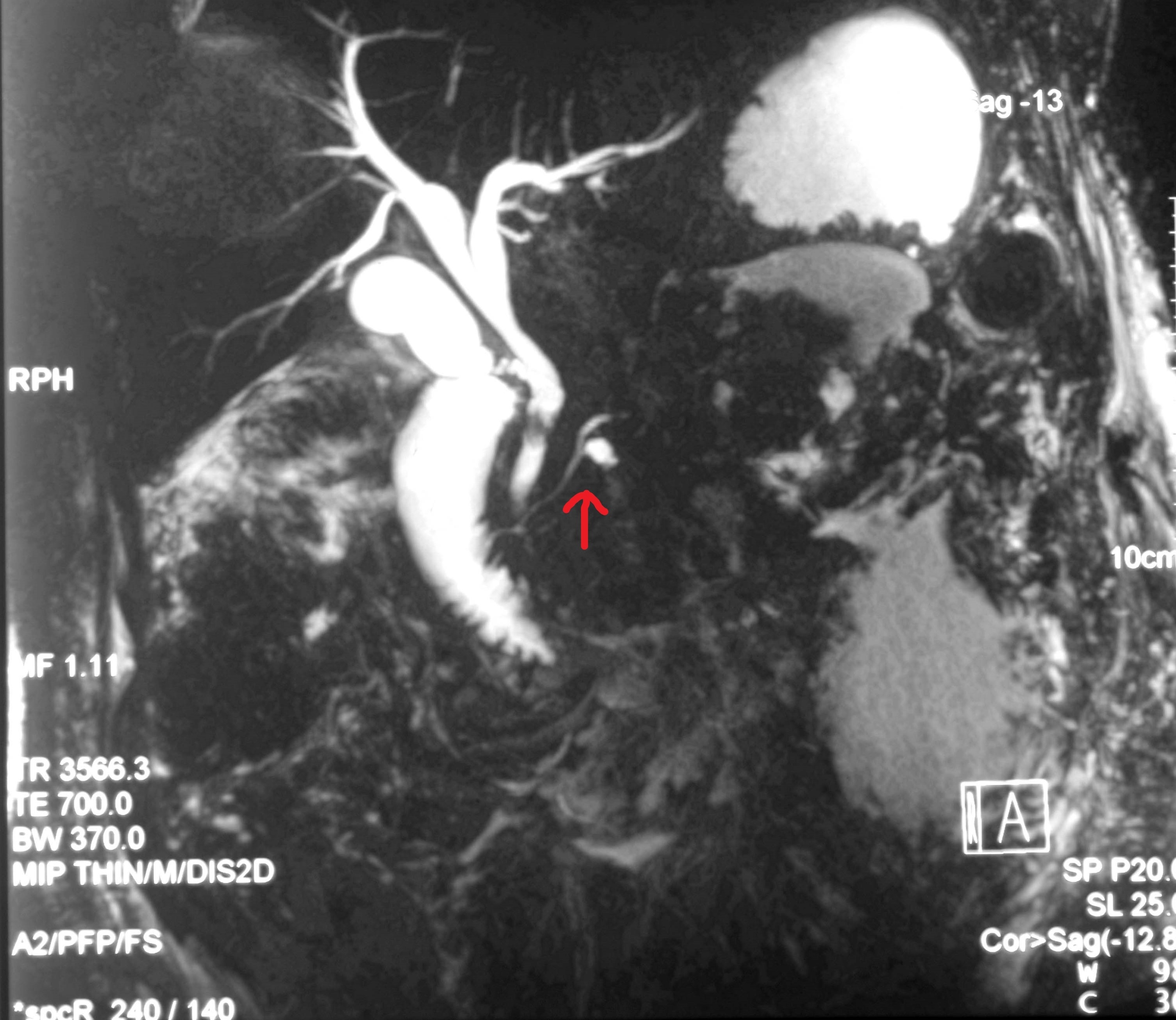
MRCP images shows disruption of MPD with two hypointense filling
defect in intrapancreatic common bile duct
Back to 2019 Abstracts




