LINEAR SUPPORT VECTOR MACHINE LEARNING MODEL IS HIGHLY SPECIFIC FOR PREDICTING LOW-GRADE INTRADUCTAL PAPILLARY MUCINOUS NEOPLASM LESIONS
Yasmin G. Hernandez-Barco*1, Dania Daye3, Jessica McGoldrick1, Keith D. Lillemoe2, Dushyant Sahani3, Brenna Casey1, David P. Ryan4, Cristina R. Ferrone2, Carlos Fernández-del Castillo2, Motaz Qadan2
1Gastroenterology, Massachusetts General Hospital, Boston, MA; 2Surgery, Massachusetts General Hospital, Boston, MA; 3Radiology, Massachusetts General Hospital, Boston, MA; 4Hematology/Oncology, Massachusetts General Hospital, Boston, MA
Background: Artificial intelligence (AI) computer-based learning modalities are being used to assist physicians in patient care. Intraductal Papillary Mucinous Neoplasm (IPMN) is a potential precursor lesion to pancreatic cancer. There are several pancreatic cyst management guidelines, including the 2015 American Gastroenterological Association (AGA) guidelines, the 2017 Revised Fukota International Consensus Guidelines (ICG) guidelines, and the American College of Gastroenterology (ACG) Guidelines for cyst management. Despite careful adherence to guidelines, our ability to accurately predict low-grade, high-grade, and invasive disease remains imperfect. We aimed to build a machine-learning tool to better predict patients with low-grade disease who may be able to avoid pancreatic resection.
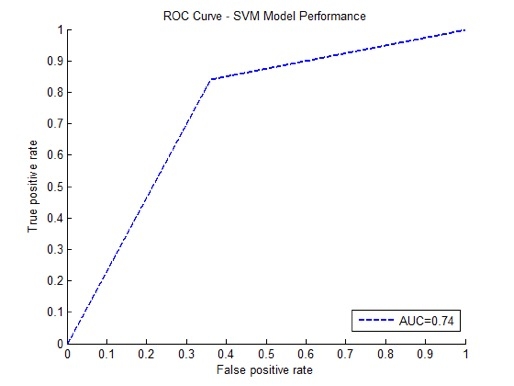
Methods: We built a linear support vector machine (SVM) learning model and analyzed a database of 575 patients who had resected IPMN. Input variables for the model included presence of jaundice, pancreatitis, gender, ethnicity, family history, personal cancer history, abdominal pain, diabetes, steatorrhea, thrombophlebitis, and CA19-9. It also included cyst characteristics such as multiloculated cysts, septations, nodularity, location, pancreatic ductal dilation, cyst size, and surgical pathology grade. Output was defined as presence of low-grade or non-low grade IPMN. The model was classifier-trained and tested using 10-fold cross-validation to avoid overfitting. ROC analysis was used to assess classification performance (Figure 1).
Results: 575 patients with pancreatic cysts were identified; mean age 68, 48.8% were male, 38.0% had lesions in the pancreatic head, 19.8% had a mural nodule, 48.5% had pancreatic ductal dilation, 27.0% had a multicystic lesion, 21.2% experienced pancreatitis, and 21.6% had diabetes. Of 575 patients who underwent surgical resection, 15.3% had low-grade dysplasia on final pathology.
After training our model using 10-fold cross-validation, a linear SVM learning model achieved 68% accuracy, with a positive predictive value of 84% and specificity of 95% in predicting low-grade dysplasia in patients with IPMN. Our results show that our SVM learning model is able to predict low-grade lesions with an AUC of 0.74 (Figure 2).
Conclusions: A linear SVM learning model can predict low-grade dysplasia with high specificity and may help further stratify which patients will need surgical resection versus ongoing surveillance.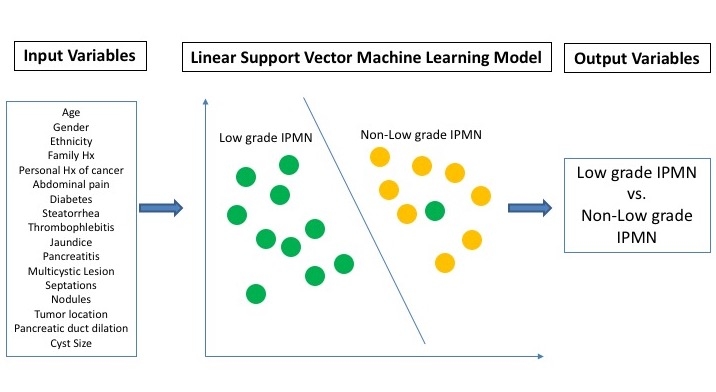
Back to 2019 Abstracts




