CLINICAL SCORES BETTER CORRELATE WITH COMPLICATION RATE IN CROHN'S DISEASE PATIENTS UNDERGOING GASTROINTESTINAL SURGERY THAN NSQIP OR ENDOSCOPIC SCORES
Kenneth D. Allen*1, Kevin R. McMahon2, Anita Afzali3, Syed Husain4
1Internal Medicine, The Ohio State University, Columbus, OH; 2School of Medicine, The Ohio State University, Columbus, OH; 3Internal Medicine/Gastroenterology, Hepatology, and Nutrition, The Ohio State University, Columbus, OH; 4Surgery/Colon and Rectal Surgery, Ohio State University, Columbus, OH
Introduction
The ACS NSQIP score was developed to predict risk in patients undergoing surgery. While commonly utilized by colorectal surgeons planning to perform gastrointestinal (GI) surgeries on patients with Crohn's Disease (CD), CD is not included in the calculator. The Harvey Bradshaw Index (HBI) and the Crohn's Disease Activity Index (CDAI) are two commonly used clinical scores for CD severity, and the Simple Endoscopic Score for Crohn's Disease (SES-CD) is a common endoscopic severity score. Considering CD is a known independent risk factor for poor surgical outcome, we hypothesize that CD severity scores will better correlate with rates of surgical complication than NSQIP score.
Methods
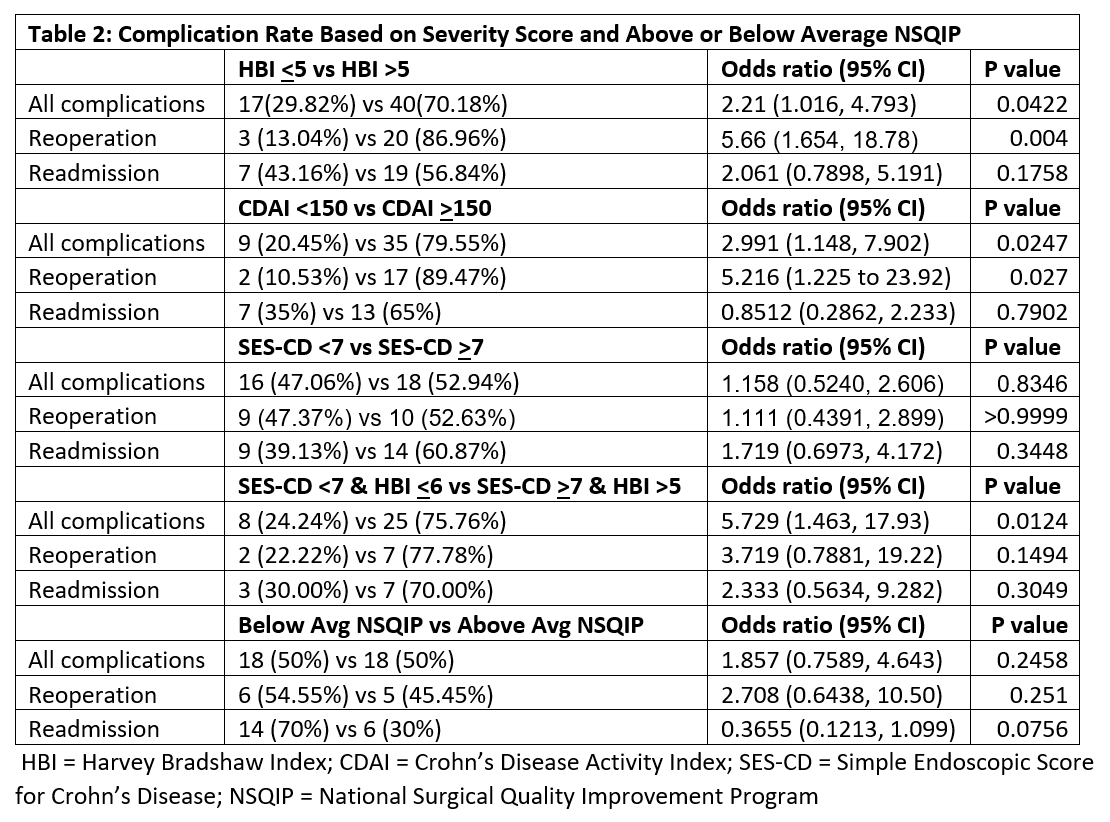
We performed a retrospective chart review of patients with CD who underwent GI surgeries from 2011 to 2017. HBI and CDAI were calculated no more than 30 days prior to surgery. SES-CD scores were calculated no more than 90 days prior to surgery. The ACS NSQIP surgical risk calculator was utilized to calculate surgical risk. Patients with HBI, CDAI, and SES-CD were all divided into moderate-high and low disease activity groups based on the respective scores (Table 2). Patients were also divided into above average and below average risk based on calculated NSQIP score. Chi-square, Fisher's exact test, and unpaired t-test were used for statistical analysis. P-value <0.05 was considered statistically significant.
Results
The HBI group included 121 patients, along with 90 CDAI patients and 103 patients with an SES-CD. NSQIP score was calculated for the 121 HBI patients. The overall complication rate was 47%. There was no significant difference in age, steroid use, or ASA class between moderate-high and low groups for any disease scores or between the two NSQIP groups. There were more males with moderate-high disease activity based on CDAI (p=0.0382), however there was no difference noted in the other groups. Patients with moderate-high disease activity had a higher complication rate for both HBI [17 vs 40 (OR = 2.21; 95% CI; 1.016, 4.793)] and CDAI [9 vs 35 (OR = 2.991; 95% CI; 1.148, 7.902)], while SES-CD showed no difference (Table 2). These groups also demonstrated an increased rate of reoperation for both HBI [3 vs 20 (OR = 5.66; 95% CI; 1.654, 18.78)] and CDAI [2 vs 17 (OR = 5.216; 95% CI; 1.225, 23.92)]. There was no significant difference in the rate of complication, reoperation, or readmission between the high and low NSQIP groups. Mean HBI and NSQIP were higher for patients who experienced any complication. Mean HBI and CDAI were higher in patients who underwent reoperation (Table 1).
Conclusion
Clinical disease severity scores for CD correlate better with surgical outcomes than NSQIP. Larger multi-center studies are necessary to further validate this finding, and these data could prove useful in developing models for predicting surgical risk in CD patients.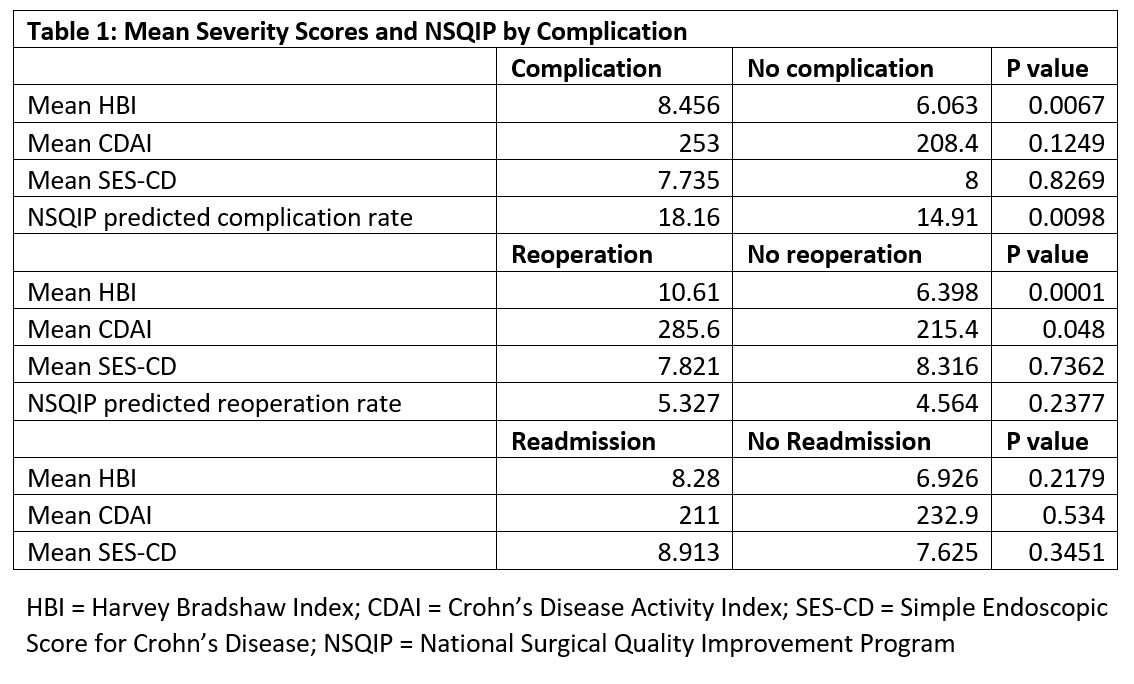
Back to 2019 Abstracts




